Nikhil Prasad Fact checked by:Thailand Medical News Team Aug 03, 2024 8 months, 3 weeks, 2 days, 12 hours, 15 minutes ago
COVID-19 News: Sudden Vision Loss Post COVID-19 Infection
In a compelling case from Japan, a 53-year-old woman experienced a sudden decrease in visual acuity just days after contracting COVID-19. This
COVID-19 News report explores the findings of researchers from the National Defense Medical College in Saitama, Japan, detailing the patient's journey and the intricate immune responses observed.
 COVID-19 infection linked to rare vision loss, a case study
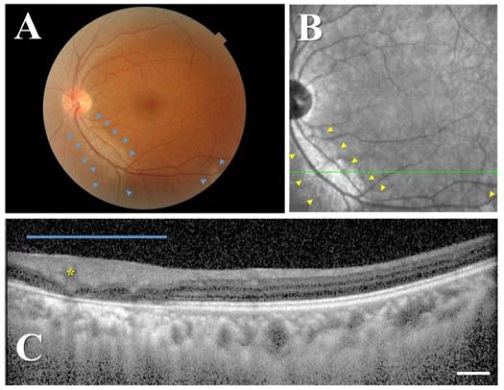
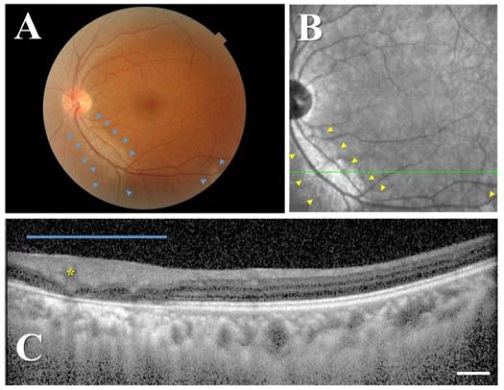
Fundus findings and visual field results of the left eye in the acute phase. (A) Color fundus photograph shows absence of retinal pigment along the inferior arcade vessels extending from the disk in the posterior retina (areas enclosed by blue arrowheads), suggesting perivascular chorioretinal atrophy associated with COVID-19. (B) Red-free fundus photograph and (C) cross-sectional EDI-OCT image of the retina along the green line. Retinal lesion is enclosed by yellow arrowheads. The blue bar indicates the extent of the lesions, and the yellow asterisk highlights a retinal blood vessel. The outer retinal layers are thinned, and the retinal layers are indistinguishable. The ellipsoid zone (photoreceptor layer) in the outer retinal layer is absent. Scale bar (white horizontal bar): 200 μm.
Case Presentation
COVID-19 infection linked to rare vision loss, a case study
Fundus findings and visual field results of the left eye in the acute phase. (A) Color fundus photograph shows absence of retinal pigment along the inferior arcade vessels extending from the disk in the posterior retina (areas enclosed by blue arrowheads), suggesting perivascular chorioretinal atrophy associated with COVID-19. (B) Red-free fundus photograph and (C) cross-sectional EDI-OCT image of the retina along the green line. Retinal lesion is enclosed by yellow arrowheads. The blue bar indicates the extent of the lesions, and the yellow asterisk highlights a retinal blood vessel. The outer retinal layers are thinned, and the retinal layers are indistinguishable. The ellipsoid zone (photoreceptor layer) in the outer retinal layer is absent. Scale bar (white horizontal bar): 200 μm.
Case Presentation
The patient, a middle-aged Japanese woman, was referred to the hospital after noticing significant vision loss following her COVID-19 diagnosis. Having received three doses of the Pfizer-BioNTech mRNA COVID-19 vaccine, her last dose was approximately seven months prior to her current illness. On the fourth day after symptom onset, she experienced a sudden drop in visual acuity in both eyes, which coincided with the resolution of her fever. At the acute phase, her best-corrected visual acuity (BCVA) was measured at 0.5 in both eyes.
Initial Findings and Diagnosis
Upon examination, color fundus photography revealed perivascular chorioretinal atrophy with peripheral pigment loss. This condition resembled pigmented paravenous chorioretinal atrophy (PPCRA). Optical coherence tomography (OCT) indicated thinning and blurred boundaries of the outer retina in the lesion sites, suggesting anatomical damage. Despite the severity of her symptoms, the patient was monitored without systemic medications.
Comprehensive Immune Profiling
Researchers conducted an in-depth analysis of the patient's immune response using advanced techniques such as mass cytometry. This method allowed them to classify leukocytes into 37 distinct immune cell types based on differentiation, function, and maturation stage. The study revealed that during the acute phase, monocytes and basophils were dominantly elevated, indicating the activation of innate immune responses to SARS-CoV-2 and allergic inflammation.
Immune Response Evolution
In the remission phase, approximately 15 weeks after the initial presentation, the patient's BCVA improved
to 0.6 in the right eye and 0.8 in the left eye. Visual field defects were partially resolved, and the anatomical structure of the outer retinal layers had recovered. The immune profiling during this phase showed an increase in Th2-like cells, plasmablasts, and neutrophils, suggesting the maturation of adaptive immunity and the preparedness of the innate immune system to combat the infection.
Insights into Cytokine Levels
The study also measured the levels of 27 cytokines in the patient's aqueous humor (AH) and serum. During the acute phase, the AH levels of certain cytokines were relatively high, indicating an immunosuppressive response in the context of perivascular chorioretinal atrophy. In contrast, serum cytokine levels were elevated, suggesting a heightened systemic immune response to SARS-CoV-2.
Hierarchical Cluster Analysis
Hierarchical cluster analysis further classified the patient's peripheral blood leukocytes into distinct groups based on similarity. This analysis identified three principal clusters, highlighting the dynamic changes in the patient's immune response from the acute phase to remission. The expression levels of specific immune cell clusters varied significantly between the two phases, reflecting the evolving nature of the immune system's battle against the virus.
Discussion and Broader Implications
The case highlights the potential for COVID-19 to cause serious ocular complications, even in patients with mild symptoms. The observed immune responses provide valuable insights into how the body reacts to the virus at different stages of infection. The detailed immune profiling and cytokine analysis offer a comprehensive understanding of the systemic and localized immune reactions in such cases.
PPCRA, typically presenting bilaterally and symmetrically, is an uncommon form of chorioretinal atrophy characterized by perivenous aggregations of pigment clumps. The case presented here suggests that COVID-19 could potentially trigger similar retinal complications. The study underscores the need for further research to explore the link between COVID-19 and ocular manifestations.
Conclusions
This case study from Japan provides a rare glimpse into the potential ocular complications associated with COVID-19. The detailed immune profiling and cytokine analysis offer a comprehensive understanding of the systemic and localized immune responses. While the patient’s visual acuity improved over time, the case underscores the importance of monitoring COVID-19 patients for potential vision-related issues. The findings contribute to the growing body of knowledge on the varied manifestations of COVID-19 and highlight the need for ongoing research in this area.
The study findings were published in the peer-reviewed journal: Vaccines.
https://www.mdpi.com/2076-393X/12/8/878
For the latest
COVID-19 News, keep on logging to Thailand Medical News.
Read Also:
https://www.thailandmedical.news/news/breaking-even-mild-covid-19-can-cause-microvasculature-changes-of-the-optic-nerve
https://www.thailandmedical.news/news/researchers-warn-that-sars-cov-2-can-infect-the-meibomian-glands-of-the-eyes