Nikhil Prasad Fact checked by:Thailand Medical News Team Apr 10, 2025 2 days, 15 hours, 41 minutes ago
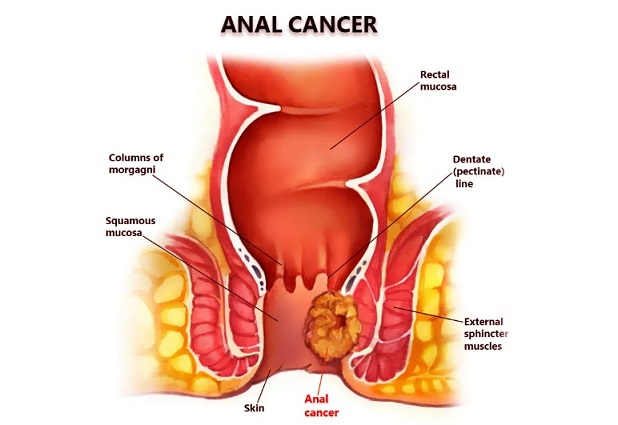
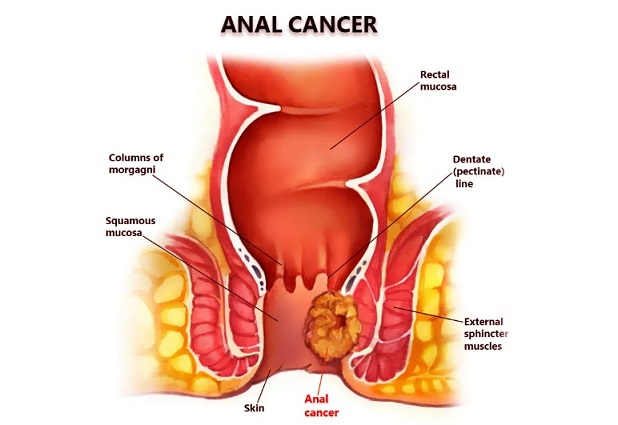
Medical News: Scientists are increasingly concerned that COVID-19 infections may be linked with a higher risk of anal cancer. While SARS-CoV-2 (the virus causing COVID-19) is not a classic cancer-causing virus, emerging research suggests it can contribute to cancer development through indirect mechanisms. We already know via various peer published studies that the SARS-CoV-2 virus especially the newer strains and lineages have enhanced tropism towards the various types of cells in the gastrointestinal tract and that viral persistence in the various ‘compartments’ of the gastrointestinal tract is prevalent.
 COVID-19 Infections Are Possibly Increasing the Risk of Anal Cancer
COVID-19 Infections Are Possibly Increasing the Risk of Anal Cancer
Various health agencies are reporting an increase in the incidences of anal cancer over the last few years, with disproportionately higher mortality in cancer patients who had COVID-19. Such observations have prompted investigations into how COVID-19 or more specifically how the SARS-CoV-2 virus might facilitate cancers like anal cancer, which is usually rare but primarily driven by chronic human papillomavirus (HPV) infection.
Emerging Clinical Evidence of a COVID-Anal Cancer Link
This
Medical News report examines recent findings that support a correlation between COVID-19 and anal cancer risk. One groundbreaking report from Spain described an unusual cluster of anal and lower rectal cancers occurring shortly after the COVID-19 pandemic. Over a two-year period, six patients with inflammatory bowel disease (IBD) developed ano-rectal malignancies, and strikingly, all tumors tested positive for SARS-CoV-2.
The presence of viral proteins in every tumor suggests the virus had persisted in the tissue or triggered changes conducive to cancer. Researchers hypothesize that inflammation related to SARS-CoV-2 infection can fuel cancer cell proliferation, even if the virus isn’t directly transforming cellsthreadreaderapp.com. These clinical observations are preliminary, but they underscore a worrying trend and echo oncologists’ reports of more aggressive cancers post-COVID.
Another hint of a link comes from HPV-related cancers. Anal cancer is often caused by persistent infection with high-risk HPV. Doctors in Germany recently documented a case of rapid progression of cervical pre-cancer to invasive cancer following a COVID-19 infection. In that case, the patient’s immune system was severely impaired after COVID-19, with sharp declines in lymphocytes and natural killer cells. The authors concluded that COVID-19 likely “exhausted” the immune system, reducing immune surveillance on the HPV-infected cells and enabling rapid cancer development. This alarming case in cervical tissue (which, like anal tissue, is HPV-driven) suggests a similar risk for accelerated anal cancer progression in patients who have had COVID-19.
Immune System Compromise and HPV Reactivation
A key mechanism behind this correlation is thought to be COVID-19’s impact on the immune system. Severe COVID-19 can cause profound inflammation and immune dysfunction
, including T-cell exhaustion and reduced counts of critical immune cells. Persistent HPV infections normally are kept in check by the immune system, but a SARS-CoV-2 infection may temporarily weaken this immune surveillance. Researchers observed in the above case study that after COVID-19, the patient’s immune cells (like T cells and NK cells) were depleted, creating an opportunity for the HPV-related lesion to progress. HPV can sometimes lie dormant or cause only minor lesions for years; a compromised immune response might reactivate latent HPV or allow existing dysplastic cells to escape immune control, hastening their progression to cancer. Essentially, COVID-19 may mimic some effects of HIV (another immunosuppressive virus) in terms of cancer risk – for example, people with HIV have much higher anal cancer rates due to immune weakness, and a bout of COVID-19 might similarly elevate short-term risk in vulnerable individuals.
Moreover, chronic COVID-19-related inflammation could aid HPV in creating a tumor-friendly environment. Inflammatory cytokines like interleukin-6 (often elevated in severe COVID) can promote cell proliferation and angiogenesis (new blood vessel growth), processes that support tumor growth. Scientists have hypothesized that the cytokine “storm” in COVID-19 exacerbates the inflammatory milieu around cells, potentially accelerating the development of cancers in tissues already harboring oncogenic viruses. Thus, HPV-driven anal pre-cancers might progress faster under the twin assault of HPV and SARS-CoV-2-induced inflammation.
Viral Oncogenic Mechanisms of SARS-CoV-2
Beyond immune effects, SARS-CoV-2 may also act directly on cellular pathways to foster cancer development. Molecular studies have revealed that SARS-CoV-2 proteins can interfere with the body’s normal tumor suppressor mechanisms. For instance, a recent review noted that the virus encodes several proteins that alter key signaling pathways associated with the hallmarks of cancer. Unlike classical cancer-causing viruses (which insert oncogenes into host cells), SARS-CoV-2 seems to promote tumorigenesis by inhibiting tumor suppressor genes and activating signals for cell survival, proliferation, and inflammation. Laboratory research confirms multiple interactions between SARS-CoV-2 proteins and human proteins that regulate cell growth and DNA repair. These interactions can tip the balance toward uncontrolled growth. For example, some studies found that the virus’s proteins can degrade p53 (a crucial tumor suppressor) and hyperactivate pathways like NF-κB and STAT3, which drive inflammation and cell division in cancers.
These biological findings raise the possibility that SARS-CoV-2 could act as an “oncovirus” or cancer facilitator, especially in tissues already at risk. It is important to note that SARS-CoV-2 likely does not directly mutate DNA to cause anal cancer. Instead, it lowers the body’s defenses and perturbs cellular environments in ways that existing cancer-causing factors (like HPV, chronic inflammation, or other carcinogens) can exploit. The result may be faster tumor growth or the appearance of cancers earlier than expected. Oncologists have indeed reported unusually aggressive tumor behavior in the post-COVID period, including cases of cancers “waking up” from dormancy and metastasizing quickly in patients who recently recovered from COVID-19. Such reports span several tumor types and regions, suggesting a systemic effect of the infection on the body’s cancer controls.
Global Health Implications and Ongoing Research
From a global perspective, these findings are prompting a re-evaluation of cancer surveillance in the wake of the pandemic. Anal cancer is already a cancer of concern, with incidence rising in many countries even before COVID-19. The pandemic may exacerbate this trend in multiple ways. First, as discussed, a COVID-19 infection might increase individual risk for anal cancer through immune suppression and inflammatory effects. Second, the pandemic disrupted routine healthcare services, including screenings for anal dysplasia and HPV vaccinations.
Public health data show that HPV vaccination rates plummeted during the COVID-19 pandemic, undoing years of progress in prevention—globally, over a quarter of HPV vaccine coverage achieved in 2019 was lost by 2021. This decline means more people worldwide remain unprotected against HPV. Fewer screenings and delayed treatments during lockdowns have similarly been reported, potentially allowing more HPV-related lesions to progress unnoticed.
Health institutions like the World Health Organization (WHO) and national cancer societies are now vigilant about these indirect effects. The WHO has warned that backsliding on HPV immunization could lead to a future surge in HPV-related cancers, including cervical and anal cancerswho.int. Meanwhile, researchers are calling for long-term studies to track cancer incidence in COVID-19 survivors.
Large cohort studies and cancer registries worldwide are being analyzed to detect any uptick in anal cancer cases that might be statistically linked to prior COVID-19 infection. Early evidence from genetic studies (e.g., Mendelian randomization analyses) indeed suggests COVID-19 might have a causal effect on increasing certain cancer risks (notably some gastrointestinal cancers), lending credence to the concern.
In summary, while it’s too early to draw definitive conclusions, there is a growing scientific consensus that COVID-19 infections can indirectly increase the risk of anal cancer. Immune system compromise, HPV reactivation, and virus-driven inflammation appear to be the main culprits underlying this link. Clinicians around the world are advised to be aware of these risks – for example, to ensure that patients recovering from severe COVID-19 catch up on cancer screenings (such as anal Pap tests for high-risk groups) and stay up-to-date with HPV vaccinations. Ongoing research will continue to clarify this COVID-cancer connection. For now, the emerging evidence underscores yet another serious long-term consequence of the COVID-19 pandemic on global health.
References:
https://academic.oup.com/ecco-jcc/article/19/Supplement_1/i757/7967367
https://biosignaling.biomedcentral.com/articles/10.1186/s12964-024-01818-0
https://www.ajmc.com/view/kashyap-patel-md-sees-link-between-covid-19-and-cancer-progression-calls-for-more-biomarker-testing
https://www.mdpi.com/1999-4915/16/8/1266
https://journals.lww.com/eurojgh/citation/2022/08000/sars_cov_2_infection_as_a_potential_trigger_factor.11.aspx
https://www.sciencedirect.com/science/article/pii/S0300908423001360?via%3Dihub
https://www.sciencedirect.com/science/article/abs/pii/S092544392400557X
https://academic.oup.com/cid/article/73/3/361/5868547
https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2023.1260776/full
https://turkjsurg.com/articles/doi/turkjsurg.2024.6494
https://surgicalcasereports.springeropen.com/articles/10.1186/s40792-024-02026-1
https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2021.804804/full
https://www.oncotarget.org/2024/05/09/sars-cov-2-spike-protein-disrupts-p53-tumor-suppressor-pathway/
https://onlinelibrary.wiley.com/doi/10.1002/jmv.28722
https://www.sciencedirect.com/science/article/pii/S0165037822002923
https://www.cancer.org/cancer/types/anal-cancer/about/what-is-key-statistics.html
https://hollingscancercenter.musc.edu/news/archive/2022/11/28/hollings-cancer-scientist-shines-the-light-on-rapid-rise-in-anal-cancer-in-us
https://www.who.int/news/item/15-07-2022-covid-19-pandemic-fuels-largest-continued-backslide-in-vaccinations-in-three-decades
For the latest COVID-19 News, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/can-sars-cov-2-cause-anal-dysplasia
https://www.thailandmedical.news/news/can-sars-cov-2-especially-the-omicron-variant-cause-hpv-and-oncogenic-hpv-reactivation-urgent-studies-warranted-based-on-growing-incidences
https://www.thailandmedical.news/articles/coronavirus
https://www.thailandmedical.news/pages/thailand_doctors_listings