COVID-19 Infections Can Lead To Spinal Cord Injuries And Myelopathies With Initial MRI Findings Showing Atypical Presentations At Onset!
Nikhil Prasad Fact checked by:Thailand Medical News Team Mar 06, 2024 1 year, 1 month, 1 week, 5 days, 4 hours, 37 minutes ago
COVID-19 News: The ongoing COVID-19 pandemic has revealed an array of clinical manifestations, extending beyond the respiratory system. Among the myriad complications associated with the virus, a growing body of evidence suggests a link between COVID-19 infections and spinal cord injuries, leading to myelopathies. This
COVID-19 News report delves into a comprehensive report from Tongren Hospital, Shanghai Jiaotong University School of Medicine, China, highlighting four cases of COVID-19-associated myelopathies. Emphasis is placed on the delayed and atypical spinal cord magnetic resonance imaging (MRI) features observed in these patients, shedding light on the complexities of the disease.
 Atypical and delayed spinal cord MRI features of COVID-19-associated myelopathies
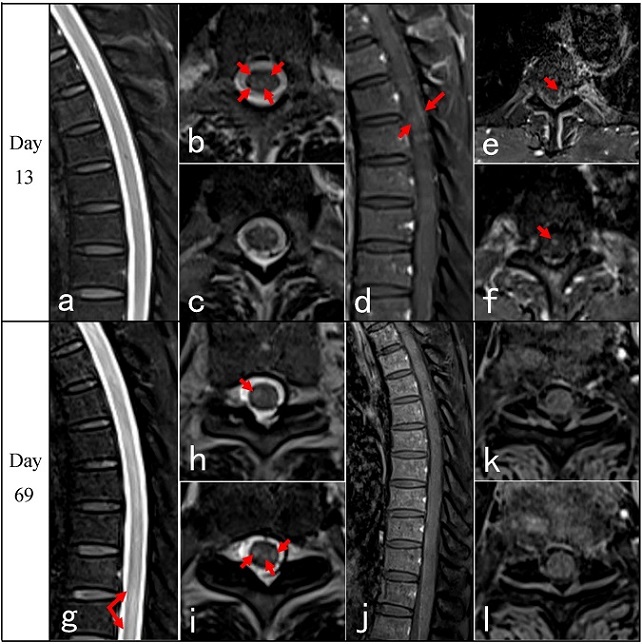
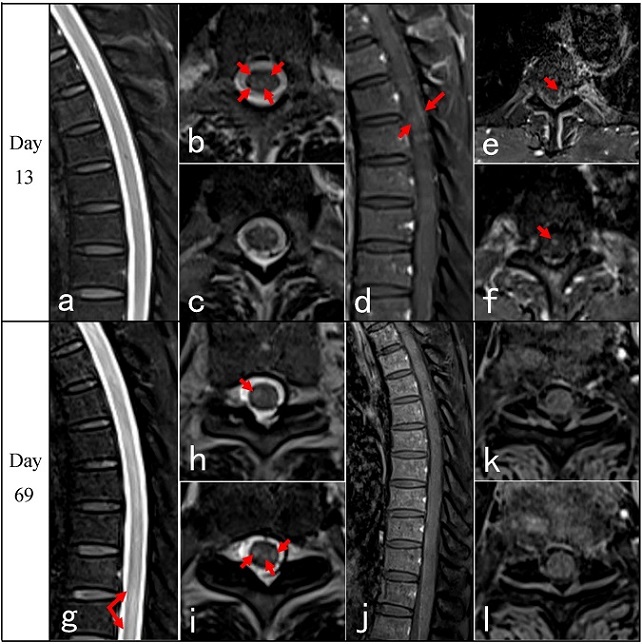
Thoracic spinal cord MRI of case 1: On day 13 from the onset, sagittal T2 did not show any abnormal signal (a). Axial T2 revealed spots-like hyperintensity (b and c, red arrows). Sagittal T1 + gadolinium showed intermittent meningeal enhancement and intramedullary cloudy-like enhancement (d, red arrows). Axial T1 + gadolinium showed scattered spots-like meningeal and intramedullary enhancement (e, f, red arrows). On day 69 follow-up, sagittal T2 showed longitudinal hyperintensities (g). Axial T2 showed scattered, patchy, intense signals in bilateral tract (h, i, red arrows). Sagittal and axial T1 + gadolinium showed no enhancement was observed on the bilateral tract lesions (j–l)
Understanding the Clinical Landscape
Atypical and delayed spinal cord MRI features of COVID-19-associated myelopathies
Thoracic spinal cord MRI of case 1: On day 13 from the onset, sagittal T2 did not show any abnormal signal (a). Axial T2 revealed spots-like hyperintensity (b and c, red arrows). Sagittal T1 + gadolinium showed intermittent meningeal enhancement and intramedullary cloudy-like enhancement (d, red arrows). Axial T1 + gadolinium showed scattered spots-like meningeal and intramedullary enhancement (e, f, red arrows). On day 69 follow-up, sagittal T2 showed longitudinal hyperintensities (g). Axial T2 showed scattered, patchy, intense signals in bilateral tract (h, i, red arrows). Sagittal and axial T1 + gadolinium showed no enhancement was observed on the bilateral tract lesions (j–l)
Understanding the Clinical Landscape
The four patients under investigation were males, ranging in age from 37 to 72 years. Their myelopathies manifested with varying latencies, occurring 5, 15, 30, and 80 days after initial COVID-19 infection. The initial symptoms included numbness and weakness of the lower limbs, back pain with lower limb weakness, and eventually progressing to severe complications such as paraplegia, sphincter dysfunction, sensory disturbance, and spastic gait. The Expanded Disability Status Scale (EDSS) scores ranged from 7.5 to 9.0, indicative of substantial disability.
MRI Findings: Unraveling the Atypical Features
Remarkably, the spinal cord MRI findings at onset were delayed and atypical. Two cases exhibited no lesions, one presented with linear spinal meningeal enhancement, and another displayed punctate lesions on T2-weighted imaging (T2WI). During the follow-up period, T2WI revealed punctate, linear, and cloudy lesions in the lateral and posterior funiculus at the peak stage. Linear spinal meningeal enhancement emerged as a prominent feature, contributing to the mismatch between clinical symptoms and MRI findings. This atypical presentation raises concerns about the recognition and timely diagnosis of COVID-19-associated myelopathy, particularly in cases with delayed and unconventional spinal cord MRI features.
/>
Background: Navigating the Neurological Terrain Post-COVID-19
Neurological manifestations following COVID-19 infection encompass a spectrum of severe conditions, including encephalitis, myelitis, Guillain–Barre syndrome, and muscle diseases. The incidence of myelitis post-COVID-19 infection is notable, accounting for 1.2% of all neurological complications. Traditional transverse myelitis (TM) and COVID-19-associated myelitis, however, exhibit distinct clinical courses and MRI features. Some patients experience delayed onset, complicating diagnosis and potentially delaying treatment. Notably, the absence of abnormal spinal cord MRI presentations may serve as a predictor of poor prognosis. Recognizing these nuances is crucial for enhancing the understanding of COVID-19-associated myelopathies.
Case Presentation: Unraveling the Clinical Threads
The detailed examination of four cases from Shanghai Tongren Hospital provides valuable insights into the clinical evolution, atypical spinal cord MRI characteristics, and treatment response in COVID-19-associated myelopathies.
-Case 1: A 70-year-old male exhibited symptoms of myelopathy 12 days after mild COVID-19 infection. Linear spinal meningeal enhancement was observed on MRI, and despite treatment, the patient's condition deteriorated.
-Case 2: A 66-year-old male developed myelopathy symptoms 49 days post-mild COVID-19. Weak linear spinal meningeal enhancement was noted on MRI. Treatment, including pulse intravenous methylprednisolone and plasma exchange, did not yield significant improvement.
-Case 3: A 72-year-old male, asymptomatic for COVID-19, developed myelopathy 80 days after the infection. Atypical spinal cord lesions were observed on MRI, and the patient's condition worsened despite treatment.
-Case 4: A 37-year-old male, 54 days post-mild COVID-19, presented with myelopathy symptoms. MRI revealed scattered high signals and long-segmental cervical spinal meningeal enhancement. Treatment with intravenous methylprednisolone showed temporary improvement, but the patient's symptoms worsened.
Discussion: Unraveling the Complexities of COVID-19-Associated Myelopathies
The discussion section delves into the intricate mechanisms through which SARS-CoV-2 affects the nervous system, exploring direct and indirect pathways. The neurological manifestations of COVID-19-associated myelitis, particularly transverse myelitis, are scrutinized. The absence of established diagnostic criteria for COVID-19-associated myelitis is acknowledged, prompting a review of diagnostic levels proposed by past studies.
The cases studies extend to the varied and atypical spinal cord MRI features observed in COVID-19-associated myelopathies. Notably, linear spinal meningeal enhancement emerges as a significant characteristic, providing valuable insights for early identification. The case study series reviews related literature, emphasizing cases with atypical and negative MRI findings, identifying 10 cases of MRI-negative COVID-19-associated myelitis. The clinical characteristics, including gait disturbances, limb weakness, and sphincter dysfunction, are discussed, showcasing the diversity within this subset of patients.
Conclusion: Navigating the Road Ahead
In conclusion, this comprehensive report sheds light on the complexities of COVID-19-associated myelopathies, emphasizing the importance of recognizing atypical spinal cord MRI features. The cases presented underscore the need for vigilance in diagnosing myelopathies even months after the initial COVID-19 infection, especially when faced with delayed and unconventional MRI findings. As the medical community strives to unravel the intricate interplay between COVID-19 and neurological complications, this report contributes to the growing body of knowledge, guiding future research and clinical practices. The imperative lies in enhancing awareness, fostering early recognition, and formulating tailored therapeutic strategies for COVID-19-associated myelopathies.
The case studies were published in the peer reviewed journal: Neurological Sciences (Springer Link).
https://link.springer.com/article/10.1007/s10072-024-07351-9
For the latest
COVID-19 News, keep on logging to Thailand Medical News.