COVID-19 Latest News: Harvard Study Shows High Frequency of Thromboembolic Occurrences Despite Prophylaxis Usage Like Heparin
Source: COVID-19 Latest News Nov 01, 2020 5 years, 1 month, 4 weeks, 1 day, 7 hours, 40 minutes ago
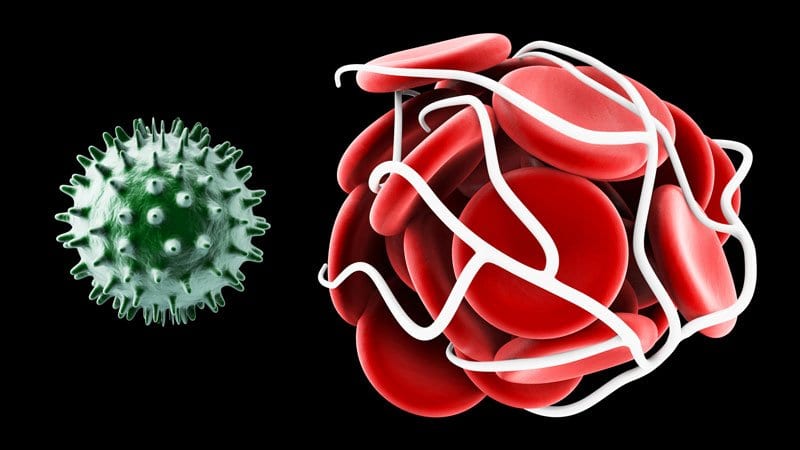
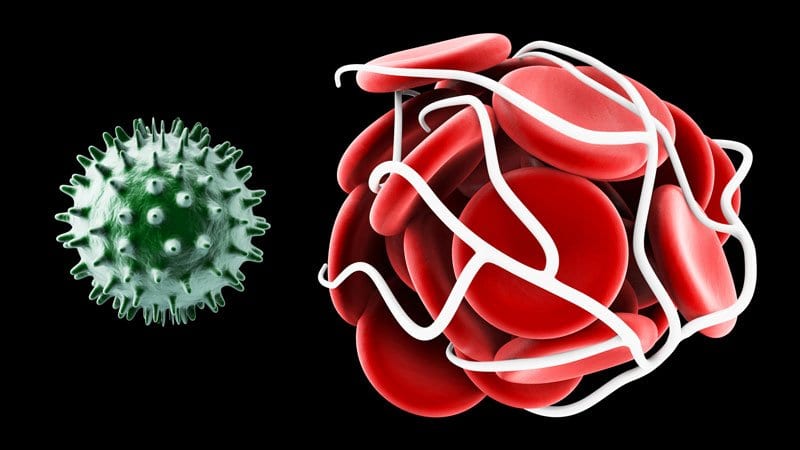
COVID-19 Latest News: Researchers from Harvard Medical School have found in a new observational study that major thromboembolic complications and adverse cardiovascular events occurred with high frequency in patients with COVID-19, especially in the intensive care setting, despite a high use of thromboprophylaxis.
The study involving a retrospective cohort of 1,114 patients with COVID-19 diagnosed through at Massachusetts General Brigham integrated health network. The total cohort was analyzed by site of care: intensive care (n = 170); hospitalized non-intensive care (n = 229); and outpatient (n = 715). The primary study outcome was a composite of adjudicated major arterial or venous thromboembolism.
COVID-19 patients in the study were 22.3% Hispanic/Latinx and 44.2% non-White. Cardiovascular risk factors of hypertension (35.8%), hyperlipidemia (28.6%), and diabetes (18.0%) were common. Prophylactic anticoagulation was prescribed in 89.4% of patients with COVID-19 in the intensive care cohort and 84.7% of those in the hospitalized non-intensive care setting. Frequencies of major arterial or venous thromboembolism, major cardiovascular adverse events, and symptomatic venous thromboembolism were highest in the intensive care cohort (35.3%, 45.9%, and 27.0 %, respectively) followed by the hospitalized non-intensive care cohort (2.6%, 6.1%, and 2.2%, respectively) and the outpatient cohort (0% for all).
The study showed that major arterial or venous thromboembolism, major adverse cardiovascular events, and symptomatic venous thromboembolism occurred with high frequency in patients with COVID-19, especially in the intensive care setting, despite a high utilization rate of thromboprophylaxis.
The study findings were published in the
Journal of the American College of Cardiology. https://www.jacc.org/doi/full/10.1016/j.jacc.2020.08.070
Lead author Dr Gregory Piazza, MD, Brigham and Women's Hospital, Boston-Massachusetts told Thailand Medical News, "Despite very high rate of antithrombotic prophylaxis there were a high rate of thromboembolic events suggesting that we are probably not providing enough thromboprophylaxis.”
He further added, "Standard prophylaxis as recommended in the guidelines is a low dose of low-molecular-weight heparin once daily, but these results suggest [patients] probably need higher doses."
Dr Piazza however cautioned that this is an observational study and randomized trials are needed to make changes in treatment strategies. Several such trials are currently underway.
The research showed that while thromboembolic complications were high, they were not as high as seen in some of the earlier studies from Asia and Europe, the study team noted.
Dr Piazza said, "The numbers we were seeing in early reports were so high we couldn't figure out how that was possible. The study suggests that in a US population receiving thromboprophylaxis, the rate of thromboembolic complications are more in line with what we would expect to see in other very sick patients who end up in ICU."
The st
udy team suggests that the very high rates of thromboembolic complications in the early studies from Asia may have been because of the lack of thromboprophylaxis, which is not routine in hospitalized patients there.
Dr Piazza explained, "Some of the earlier studies also used routine ultrasound and so picked up asymptomatic thrombotic events, which was not the case in our study. So our results are more representative of the US population.”
He attributes the high rate of thromboembolic complications being reported with COVID-19 to the sheer number of very sick patients being admitted to the hospital.
The team added, "We are accustomed to seeing a rare case of thrombosis despite prophylaxis in hospitalized patients, but we are seeing more in COVID patients. This is probably just because we have more critically ill patients. We are seeing an incredible influx of patients to the ICU that we have never experienced before, so the increase in thromboembolic complications is more obvious. In prior years we probably haven't had enough critically ill patients at any one time to raise the flag about thromboprophylaxis.”
The team also discovered a high rate of cardiovascular complications. They are seeing an increase in the risk of myocardial infarction, which is to be expected in such sick patients, but they also see quite a bit of new atrial fibrillation, myocarditis, and heart failure in patients who don't always have underlying cardiovascular disease.
Dr Paizza said, "So this virus does appear to have a predilection to causing cardiovascular complications, but this is probably because it is making patients so sick. If flu was this virulent and resulted in such high rates of acute respiratory distress syndrome (ARDS), we would probably see similar cardiovascular complication rates."
The study team analyzed a retrospective cohort of 1114 patients with COVID-19 diagnosed through the Mass General Brigham integrated health network. Of these, 170 had been admitted to the ICU, 229 had been hospitalized but not treated in ICU, and 715 were outpatients. In terms of ethnicity, 22% were Hispanic/Latinx and 44% were non-White.
The study showed that cardiovascular risk factors were common, with 36% of patients having hypertension, 29% hyperlipidemia, and 18% diabetes. Prophylactic anticoagulation was prescribed in 89% of patients with COVID-19 in the intensive care cohort and 85% of those in the hospitalized non-intensive care setting.
Study results showed that major arterial or venous thromboembolism occurred in 35% of the intensive care cohort, 2.6% of those hospitalized but not treated in ICU, and 0% of outpatients.
It was found that major adverse cardiovascular events occurred in 46% of the intensive care cohort, 6.1% of those hospitalized but non-ICU, and 0% of outpatients.
Also symptomatic venous thromboembolism occurred in 27% of those admitted to ICU, 2.2% of those hospitalized but non-ICU, and 0% of outpatients.
Dr Piazza commented, "We found that outpatients had a very low rate of thromboembolic complications, with the vast majority of the risk being in hospitalized patients, especially those in ICU." These study results suggest that we do not need routine thromboprophylaxis for all outpatients with COVID-19, but there will probably be some patients who need it ie those with risk factors for thromboembolism."
It should be noted that catheter and device-associated deep vein thrombosis (DVT) accounted for 76.9% of the DVTs observed in the research.
The study team said, "Our research finding of high frequency of catheter-associated DVT supports the judicious use of central venous catheters that have been widely implemented, especially in the ICU, to minimize recurrent health care team exposure and facilitate monitoring.”
Importantly Of all the markers of disease severity, the presence of ARDS had the strongest association with adverse outcomes, including major arterial or venous thromboembolism, major adverse cardiovascular events, symptomatic venous thromboembolism and death.
Dr Piazza said, "The severe inflammatory state associated with ARDS and other complications of COVID-19 and its resultant hypercoagulability may explain, at least in part, the high frequency of thromboembolic events. Improved risk stratification, utilizing biochemical markers of inflammation and activated coagulation as well as clinical indicators, such as ARDS, may play an important role in the early identification of patients with an increased likelihood of developing symptomatic VTE or arterial thrombosis. They may benefit from full- or intermediate-intensity antithrombotic therapy rather than prophylactic anticoagulation."
The study team points out that this study provides a cross-sectional view of the cardiovascular complications of COVID-19 in a large healthcare network, consisting of two academic medical centers serving the greater Boston area, several community hospitals, and numerous outpatient care sites.
The team said, "The study incorporates a wide scope of clinically meaningful cardiovascular endpoints and utilizes a rigorous process of event adjudication. Although data on patients with COVID-19 in the ICU have been the subject of most reports, our study provides insights into the broad spectrum of all hospitalized and outpatient populations.”
They concluded, “Arterial or venous thromboembolism and major adverse cardiovascular events were common over 30 days in ICU patients with COVID-19. ARDS was strongly associated with cardiovascular complications. Patients with COVID-19 in the hospitalized non-ICU cohort were also susceptible to cardiovascular complications, although not to the extent of those in the critical care setting. The high frequency of arterial or venous thromboembolism in hospitalized patients despite routine thromboprophylaxis suggests the need for improved risk stratification and enhanced preventive efforts.”
The research is continuing, and the study team expects to have data on 10,000 patients by the end of winter.
For more
COVID-19 Latest News, keep on logging to Thailand Medical News