COVID-19 News: Are SARS-CoV-2 Infections Leading To The Onset Of Acute Diverticulitis And Complications For Those Already With Diverticulitis?
Nikhil Prasad Fact checked by:Thailand Medical News Team Oct 08, 2023 2 years, 2 months, 1 week, 6 days, 14 hours, 30 minutes ago
COVID-19 News: In the midst of the ongoing COVID-19 pandemic, researchers have been diligently studying the various manifestations of the virus. While respiratory symptoms have dominated the headlines, the impact of SARS-CoV-2, the virus responsible for COVID-19, on the gastrointestinal system has been increasingly recognized as covered in various studies and
COVID-19 News reports.
However, one aspect that hasn't received as much attention is the potential link between COVID-19 infections and the development of acute diverticulitis, a painful condition affecting the digestive tract.
Additionally, for those who already have diverticulitis, there's been a growing concern about the exacerbation of their condition due to COVID-19.
Understanding Diverticulosis and Diverticulitis
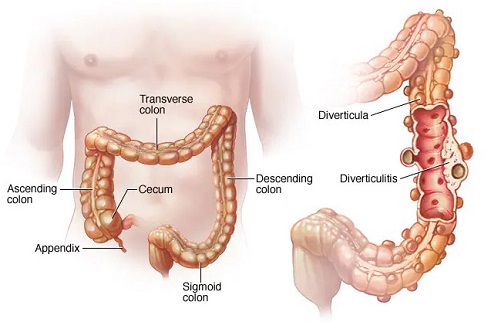
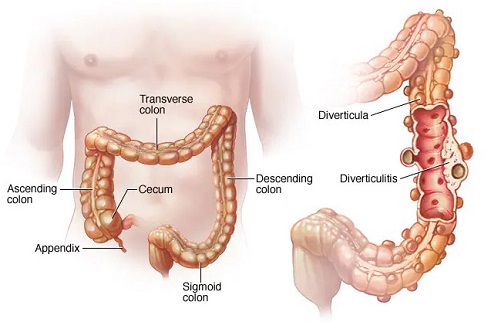
To comprehend the implications of COVID-19 on diverticulitis, it's essential to understand these conditions. Diverticulosis is a common occurrence, especially among individuals over the age of 40. It involves the formation of small pouches, known as diverticula, in the lining of the digestive system, particularly in the lower part of the large intestine or colon. These pouches typically don't cause problems by themselves.
However, when one or more of these diverticula become inflamed or infected, the condition transitions to diverticulitis. This shift can result in severe abdominal pain, fever, nausea, and changes in bowel habits. Mild cases of diverticulitis can often be managed with rest, dietary modifications, and antibiotics, while severe or recurrent cases may require surgical intervention.
The Emergence of Acute Diverticulitis Following COVID-19 Infections
Recent research, including a study conducted earlier this year by the Mayo Clinic in Jacksonville, USA, has raised concerns about the potential relationship between COVID-19 and the development of acute diverticulitis. The Mayo Clinic study focused on individuals who developed acute diverticulitis within 30 days of being diagnosed with COVID-19. It revealed a strikingly high complication rate, with intestinal perforation being the most common complication.
The study, conducted by the Department of Gastroenterology and Hepatology at Mayo Clinic, Jacksonville, USA, aimed to further characterize this association between COVID-19 and first-time acute diverticulitis within a large academic medical center. Researchers identified patients diagnosed with COVID-19 who subsequently developed acute diverticulitis within the specified timeframe. Both COVID-19 and acute diverticulitis diagnoses were confirmed using polymerase chain reaction and computed tomography, respectively.
The findings from this study shed light on the severity of complications associated with acute diverticulitis following COVID-19 infection. Among the key findings:
-
High Complication Rate: A total of 81 patients were identified, and they developed acute diverticulitis within a median duration of 13 days after their COVID-19 diagnosis. A significant 59.3% of these patients experienced complications, w
ith intestinal perforation being the most common, followed by abscess formation and peritonitis.
-Vaccination Trends: While there was a trend toward increased complications in unvaccinated COVID-19 patients, this difference didn't reach statistical significance. However, patients diagnosed with acute diverticulitis at the same time as their COVID-19 diagnosis had significantly higher rates of complications and a greater need for emergency surgery.
-Implications for Clinical Care: These findings underscore the need for heightened vigilance and monitoring of COVID-19-positive patients who develop diverticulitis, especially those diagnosed with both conditions simultaneously.
Exploring the Mechanisms Behind the Link
The link between COVID-19 and acute diverticulitis raises questions about the underlying mechanisms. COVID-19 is known to cause a systemic inflammatory response, affecting various organs and systems beyond the respiratory system. This inflammatory state is believed to be a key driver of extrapulmonary manifestations, including gastrointestinal symptoms such as nausea, vomiting, diarrhea, anorexia, and abdominal pain.
Acute diverticulitis, on the other hand, has traditionally been associated with the obstruction of intestinal diverticula by fecal matter, leading to low-grade inflammation, mucosal damage, bacterial overgrowth, and microperforation. Recent research has also linked chronic inflammatory states, alterations in the gut microbiome, and the development of acute diverticulitis.
Given these potential overlapping mechanisms, it's plausible that the generalized inflammatory response triggered by COVID-19 could predispose individuals to acute diverticulitis or exacerbate existing cases. Histopathological evidence has shown that COVID-19 infection can result in the infiltration of immune cells into the intestinal tissue, leading to endothelial inflammation, microvascular injury, and mesenteric ischemia. This combination of inflammation and ischemia could contribute to the higher incidence of complications observed in COVID-19 patients with acute diverticulitis.
Limitations and Future Research
It's important to note the limitations of this study. It was conducted retrospectively at a single academic institution, and the patient population was predominantly older and Caucasian. Future research should aim to include more diverse populations and data from multiple institutions to provide a broader understanding of this association.
In conclusion, the link between COVID-19 infections and the onset of acute diverticulitis, as well as the exacerbation of existing cases, is a concerning development. The study highlights a high complication rate in COVID-19-positive patients who develop acute diverticulitis, particularly with intestinal perforation and peritonitis. These findings emphasize the need for increased vigilance and monitoring of such patients and suggest that timely intervention may be crucial in managing their condition effectively. As the world continues to grapple with the complexities of COVID-19, ongoing research will be essential to further understand and address these emerging associations.
The study findings were published in the peer reviewed journal: Cureus.
https://www.cureus.com/articles/129904-association-between-coronavirus-disease-2019-and-acute-complicated-diverticulitis#!/
For the latest
COVID-19 News, keep on logging to Thailand Medical News.
Read Also:
Acute Perforated Diverticulitis as a Potential Complication of SARS-CoV-2 (COVID-19)
https://journals.lww.com/ajg/fulltext/2020/10001/s1625_acute_perforated_diverticulitis_as_a.1626.aspx
Abdominopelvic CT in COVID-19 patients with abdominal complaints including both waves and controls: reader agreement and overcalls after consensus review
https://www.sciencedirect.com/science/article/abs/pii/S0899707123002085
SARS-CoV-2 and acute diverticulitis: The expanding gastrointestinal manifestations of COVID-19 infection
https://www.degruyter.com/document/doi/10.2478/jtim-2021-0019/html
Meckel’s diverticulitis in a COVID-19 adult
https://academic.oup.com/jscr/article/2021/3/rjab059/6179382
Acute diverticulitis in COVID-19 patients: parallel management in three cases. Are the guidelines adapting?
https://air.unimi.it/handle/2434/898773
Clinical cases of complicated diverticulitis against the background of severe course COVID-19. Case report
https://pesquisa.bvsalud.org/global-literature-on-novel-coronavirus-2019-ncov/resource/pt/covidwho-2318335
Hospital Presentations of Acute Diverticulitis During COVID-19 Pandemic may be More Likely to Require Surgery due to Increased Severity: A Single-Centre Experience
https://journals.sagepub.com/doi/10.1177/0003134820982560
Perforation of Jejunal Diverticula in COVID-19 Positive Patients: A Case Series
https://www.jcdr.net/articles/PDF/16363/52657_CE[Ra1]_F(KR)_PF1(AG_SS)_PFA(AG_KM)_PN(KM).pdf