COVID-19 News: German And Swiss Study Finds That SARS-CoV-2-Associated T-Cell Infiltrates The Brain!
Nikhil Prasad Fact checked by:Thailand Medical News Team Feb 03, 2024 1 year, 2 months, 1 week, 6 days, 21 minutes ago
COVID-19 News: In the labyrinth of challenges posed by the COVID-19 pandemic, one intriguing facet is the connection between severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and the human brain. Beyond its primary respiratory impact, COVID-19 is revealing itself as a complex disease with neurological implications that extend far beyond the acute phase of infection. A collaborative study covered in this
COVID-19 News report conducted by esteemed institutions - the University Medical Centre Hamburg-Eppendorf in Germany, the University Hospital Basel in Switzerland, and Martin-Luther-University Halle-Wittenberg in Germany - aimed to unravel the intricate relationship between SARS-CoV-2 and the human brain, shedding light on the complexities of neuroinflammation and long-term neurological complications associated with COVID-19.
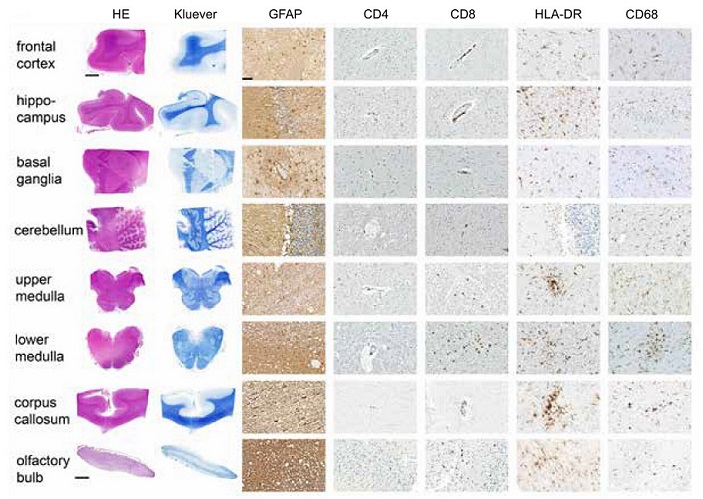
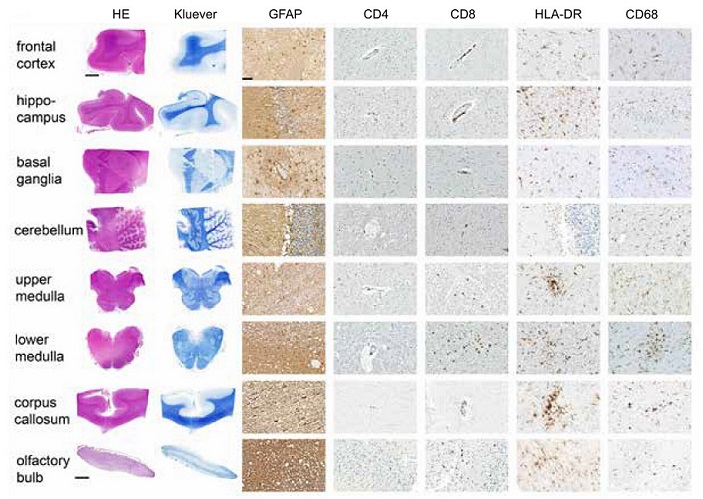 Histopathological and immunohistochemical analysis of different brain regions from COVID-19 deceased patients.
Histopathological and immunohistochemical analysis of different brain regions from COVID-19 deceased patients.
Haematoxylin & eosin- (HE) and Kluever stainings to assess general morphology and myelination status (first two columns). The remaining 5 columns show the results of the immunohistochemistry for GFAP, CD4+ and CD8+ T cells, MHC class II expression (HLA-DR) and microglia/macrophage infiltration (CD68) to assess the degree of immune infiltration and local neuroinflammation. In comparison with the hindbrain, reactive astrogliosis was more pronounced in the forebrain. Generally, perivascular CD4+ cells were very sparse, while both perivascular and parenchymal CD8+ cells were seen more frequently, especially in the medulla oblongata. The degree of microgliosis varied both between patients and regions, changing between diffuse patterns and microglial nodules
Exploring Neurological Complications
The study delves into the pathophysiology and neuropathogenesis that underlie the neurological complications observed in COVID-19 patients. While the acute phase of SARS-CoV-2 infection primarily manifests as respiratory illness, a growing number of patients experience persistent neurological symptoms, ranging from acute encephalopathy to long-term COVID-19. This long-hauler syndrome is characterized by symptoms such as fatigue, sleep disturbances, arthralgia, and breathlessness, raising questions about the virus's impact on the central nervous system (CNS).
The Intricate Role of T-Cell Infiltration
To unravel the complexities of neuroinflammation associated with COVID-19, the researchers focused their attention on T-cell infiltration into the brain. The adaptive immune response triggered by SARS-CoV-2 infection involves virus-specific T-cell activation, leading to CD8+ mediated viral clearance. The study aimed to investigate the presence of SARS-CoV-2-associated T cells in various regions of the brain and understand their potential connection to neurological symptoms, both acute and long-term.
Methodology: A Detailed Examination
The researchers employed a meticulous approach, conducting a detailed analysis of brain tissue obtained from de
ceased COVID-19 patients who succumbed to severe pneumonia or related complications. Distinct anatomical brain regions, including the olfactory bulb, medulla, cerebellum, and others, were subjected to examination using T-cell receptor Vβ repertoire sequencing (TRBV). Additionally, the study incorporated histopathological evaluations to assess T-cell infiltration patterns, with a specific focus on CD8+ T-cell involvement and a perivascular infiltration pattern.
Key Findings: A Mosaic of SARS-CoV-2-Specific T Cells
The results of the study revealed a widespread presence of SARS-CoV-2-associated T cells in almost all analyzed brain areas of patients with fatal COVID-19 courses. The olfactory bulb, medulla, and cerebellum exhibited the most distinctive SARS-CoV-2-specific sequence patterns, offering insights into the preferential targeting of these brain regions by virus-specific T cells. The study identified 103 unique clonotypes in COVID-19 specimens, emphasizing the oligoclonal infiltration of T cells throughout various brain regions.
Validation and Comparative Analysis: Bridging the Gaps
To validate their findings and provide a broader perspective, the researchers compared the identified clonotypes with blood repertoires from unrelated COVID-19 patients with active infection and healthy individuals. The clonotypes derived from specific brain regions demonstrated a higher prevalence in the blood repertoires of COVID-19 patients, indicating a potential tissue tropism towards these brain areas. Further analysis revealed similarity matches with known SARS-CoV-2-reactive T-cell clones, highlighting the potential association between these infiltrating T cells and the virus.
Morphological Assessment
The study extended its exploration to the morphological assessment of the distinct brain regions, aiming to better understand the phenotype of COVID-19-related T-cell infiltration. CD8+ T-cell infiltration emerged as predominant, supporting the notion of a virus-specific immune response. Microglia activation and reactive astrogliosis were observed, indicating an inflammatory response. The distribution of these immune cells varied across different brain regions, providing nuanced insights into the intricacies of neuroinflammation associated with COVID-19.
Discussion and Future Implications
The study aligns with existing research highlighting endothelial damage and subsequent perivascular inflammation as a key mechanism of neuroinflammation in COVID-19. While the exact role of CNS-infiltrating T cells remains unclear, the study's findings emphasize the need for future research to elucidate the mechanisms of reactive neuroinflammation, potential CNS autoimmunity, and the relationship between T-cell infiltration and neurological symptoms in COVID-19 patients.
Acknowledging Limitations and Urging Further Exploration
Despite providing strong evidence for SARS-CoV-2-specific T-cell infiltration into the brain, the study acknowledges its limitations, including the small cohort size and the necessity for further confirmation of specificity in future studies. The complex landscape of post-mortem donors, coupled with concurrent neurological diseases, adds a layer of complexity to the study's findings.
Conclusion: A Mosaic Yet to Be Fully Decoded
In conclusion, given the substantial number of people worldwide affected by SARS-CoV-2, with potential long-term sequelae of concomitant neuroinflammation, the role of CNS-infiltrating and virus-specific T cells represents a critical area for future research. While the study provides a significant step forward in unraveling the mysteries of SARS-CoV-2-associated T-cell infiltration into the brain, the small cohort size and the need for further confirmation underscore the complexity of these interactions. As the pandemic continues, this comprehensive study contributes valuable insights that may shape the future direction of research in the field of COVID-19 neurology, ultimately aiding in the development of targeted interventions and treatments for neurological complications associated with the virus.
The study findings were published in the peer reviewed journal: Clinical and Translational Immunology (Wiley).
https://onlinelibrary.wiley.com/doi/10.1002/cti2.1487
For the latest
COVID-19 News, keep on logging to Thailand Medical News.