COVID-19 News: German Study Discovers ACE2-Independent SARS-CoV-2 Virus Entry Through Cell Surface GRP78 On Monocytes!
Nikhil Prasad Fact checked by:Thailand Medical News Team Nov 15, 2023 1 year, 5 months, 5 days, 17 hours, 12 minutes ago
COVID-19 News: The global COVID-19 pandemic, caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has affected millions, presenting a complex clinical spectrum from mild respiratory symptoms to severe pneumonia and multi-organ failure. Understanding the virus's intricate mechanisms of entry into host cells is crucial for developing effective treatments.
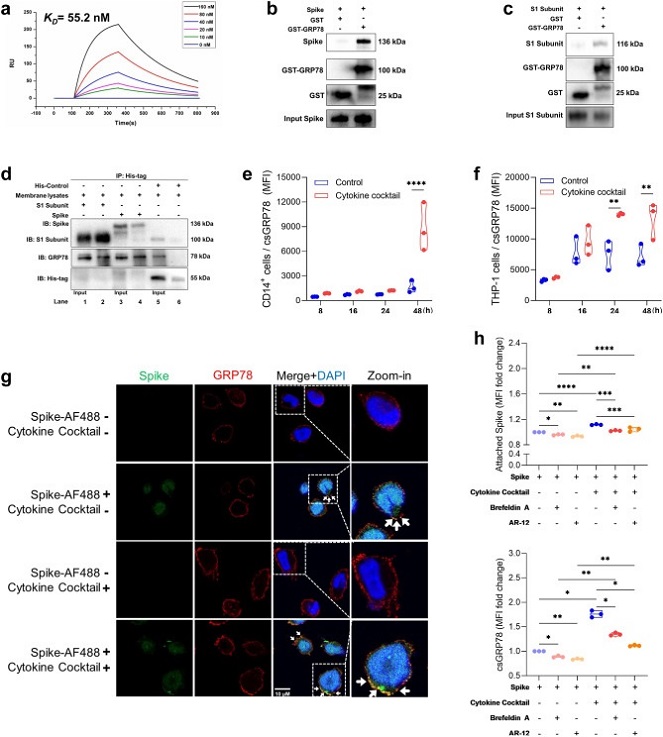
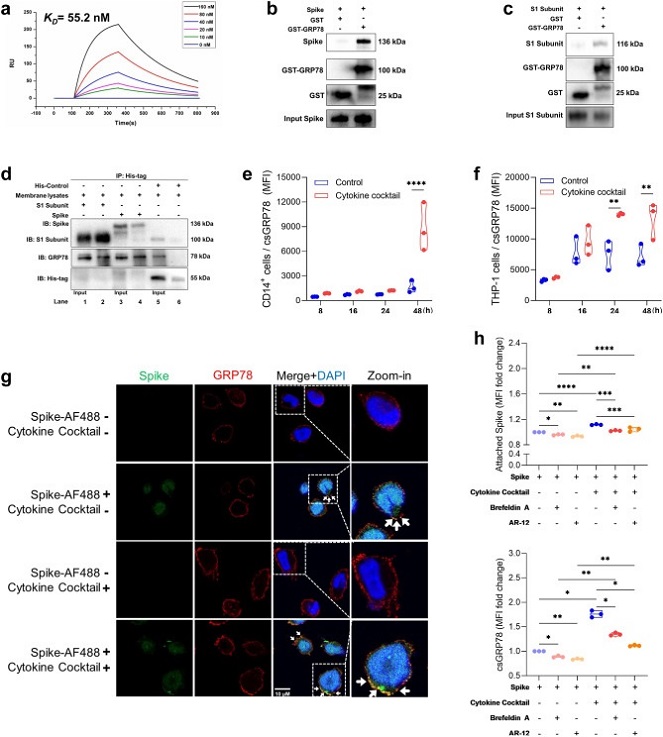 Interaction and colocalization between csGRP78 and SARS-CoV-2 spike protein. Surface plasmon resonance analysis showing the interaction intensity between GST-GRP78 and spike protein expressed as affinity constant KD = 55.2 nM (a). GST Pull-down assay showing direct interaction between GST-GRP78 with SARS-CoV-2 spike protein (b) and S1 subunit (c). Co-immunoprecipitation demonstrating GRP78 extraction together with SARS-CoV-2 S1 subunit (lane 2) and spike protein (lane 4) on THP-1 cell membrane (d). Cytokine cocktail (IL-1β, IL-6, TNF and IFN-γ) induced csGRP78 expression (MFI) on CD14+ monocytes derived from PBMCs from healthy donors (n = 3) (e) and on THP-1 cells (n = 3) (f) over time course of 48 h. Representative immunofluorescence staining from triplicates of SARS-CoV-2 spike protein (green) and csGRP78 (red) in THP-1 cells before and after cytokine cocktail stimulation for 48 h. Arrows indicate colocalization. Scale bar 10 μm (g). Flow-cytometric analysis of spike protein adhesion (upper chart), and csGRP78 expression (lower chart) on THP-1 cells after 48 h spike protein stimulation with or without cytokine cocktail, brefeldin A (0.03 μg/ml) or AR-12 (5 μM), presented as fold change (h). Violine plots indicate median values and interquartile range. Statistical differences between two groups were calculated by Mann–Whitney U test and between four groups by ANOVA with Tukey multiple comparison test, ∗P < 0.05, ∗∗P < 0.01, ∗∗∗P < 0.005, ∗∗∗∗P < 0.001.
Interaction and colocalization between csGRP78 and SARS-CoV-2 spike protein. Surface plasmon resonance analysis showing the interaction intensity between GST-GRP78 and spike protein expressed as affinity constant KD = 55.2 nM (a). GST Pull-down assay showing direct interaction between GST-GRP78 with SARS-CoV-2 spike protein (b) and S1 subunit (c). Co-immunoprecipitation demonstrating GRP78 extraction together with SARS-CoV-2 S1 subunit (lane 2) and spike protein (lane 4) on THP-1 cell membrane (d). Cytokine cocktail (IL-1β, IL-6, TNF and IFN-γ) induced csGRP78 expression (MFI) on CD14+ monocytes derived from PBMCs from healthy donors (n = 3) (e) and on THP-1 cells (n = 3) (f) over time course of 48 h. Representative immunofluorescence staining from triplicates of SARS-CoV-2 spike protein (green) and csGRP78 (red) in THP-1 cells before and after cytokine cocktail stimulation for 48 h. Arrows indicate colocalization. Scale bar 10 μm (g). Flow-cytometric analysis of spike protein adhesion (upper chart), and csGRP78 expression (lower chart) on THP-1 cells after 48 h spike protein stimulation with or without cytokine cocktail, brefeldin A (0.03 μg/ml) or AR-12 (5 μM), presented as fold change (h). Violine plots indicate median values and interquartile range. Statistical differences between two groups were calculated by Mann–Whitney U test and between four groups by ANOVA with Tukey multiple comparison test, ∗P < 0.05, ∗∗P < 0.01, ∗∗∗P < 0.005, ∗∗∗∗P < 0.001.
Recent groundbreaking research conducted by the LMU Hospital in Germany, the Institute of Lung Health and Immunity at Helmholtz Zentrum München, and Ludwig-Maximilians-Universität in Munich covered in this
COVID-19 News report, reveals a novel avenue of SARS-CoV-2 infection. The study uncovers a previously unknown entry mechanism involving the cell surface glucose-regulated protein 78 (csGRP78) on monocytes, shedding light on the virus's ability to infect cells independent of the well-established ACE2/TMPRSS2 pathway.
Background
SARS-CoV-2 primarily enters respiratory epithelial cells through the angiotensin-converting enzyme 2 (ACE2) receptor, facilitated by the transmembrane serine protease 2 (TMPRSS2). However, monocytes and macrophages, crucial players in severe COVID-19 cases, express low or negligible levels of ACE2, suggesting alternative entry routes for these immune cells. In silico analyses had earlier predicted that csGRP78, a protein constitutively expressed on monocytes and macrophages, could serve as a potential receptor for SARS-CoV-2.
Methods
Th
e study focused on hospitalized COVID-19 patients, characterizing their pro-inflammatory state and csGRP78 expression on monocytes in comparison to healthy controls. Transcriptome analyses of CD14+ monocytes, bioinformatic re-analyses of bronchoalveolar lavage fluid (BALF) datasets, and immunohistocytochemistry on post-mortem lung tissues were conducted. The research also involved cell culture experiments to validate the interaction between csGRP78 and the SARS-CoV-2 spike protein, determining the role of csGRP78 in ACE2-independent virus entry into monocytes.
Findings
The results unveiled a distinct pro-inflammatory state in COVID-19 patients, with elevated cytokine levels and increased csGRP78 expression on peripheral blood and lung monocytes/macrophages. The study confirmed an association between pro-inflammatory cytokines and csGRP78 upregulation. In vitro analyses demonstrated a high-affinity interaction (KD = 55.2 nM) between csGRP78 and the SARS-CoV-2 spike protein, validating csGRP78 as a receptor for the virus. Importantly, infection rate analyses in monocytes showed increased uptake of the virus, emphasizing csGRP78's role in ACE2-independent SARS-CoV-2 entry.
Interpretation
This groundbreaking research challenges the conventional understanding of SARS-CoV-2 entry, revealing csGRP78 as a crucial receptor for the virus on monocytes. The study suggests that the enhanced expression of csGRP78, driven by pro-inflammatory cytokines, mediates ACE2-independent virus entry into monocytes, contributing to hyperinflammation observed in severe COVID-19 cases. Targeting csGRP78 emerges as a potential therapeutic strategy to mitigate the hyperinflammatory response and improve patient outcomes.
Added Value
The research provides a translational approach, integrating clinical data with in vitro experiments and bioinformatic analyses. By confirming csGRP78 upregulation in COVID-19 patients and establishing its interaction with the SARS-CoV-2 spike protein, the study bridges the gap between clinical observations and molecular mechanisms. The findings offer new insights into COVID-19 pathogenesis, highlighting csGRP78 as a promising target for drug development.
Implications
This study has far-reaching implications for understanding the dynamics of SARS-CoV-2 infection, particularly in immune cells like monocytes. The identification of csGRP78 as a key player in virus entry opens avenues for targeted therapies to modulate the hyperinflammatory response seen in severe COVID-19 cases. The potential of small molecule inhibitors, such as BOLD-100, to disrupt csGRP78 upregulation presents a promising avenue for further investigation and clinical trials.
Discussion
The study's groundbreaking nature lies in unraveling a previously unknown entry mechanism for SARS-CoV-2, challenging the prevailing ACE2-centric view.
Monocytes and macrophages, pivotal in COVID-19 pathology, exhibit increased csGRP78 expression in response to pro-inflammatory stimuli. This study not only confirms the association between inflammation and csGRP78 upregulation but also establishes a direct interaction between csGRP78 and the virus. The proposed sequence of hyperinflammation involves early SARS-CoV-2 infection inducing pro-inflammatory cytokine secretion, activating the unfolded protein response in monocytes, and leading to csGRP78 upregulation. Subsequent virus entry into monocytes exacerbates the dysregulated immune response, contributing to the hyperinflammatory syndrome observed in severe COVID-19.
Conclusion
In conclusion, this study presents a paradigm shift in our understanding of SARS-CoV-2 entry into host cells. The identification of csGRP78 as a receptor for the virus on monocytes opens new avenues for therapeutic interventions to modulate the hyperinflammatory response in severe COVID-19 cases. Further research and clinical trials are warranted to explore the potential of targeting csGRP78, especially using small molecule inhibitors like BOLD-100, as a viable strategy in the fight against COVID-19. This discovery not only enriches our knowledge of the virus's pathogenesis but also provides a promising direction for the development of targeted antiviral therapies.
The study findings were published in the peer reviewed journal: eBioMedicine.
https://www.sciencedirect.com/science/article/pii/S2352396423004358
For the latest
COVID-19 News, keep on logging to Thailand Medical News.