COVID-19 News: Italian Study Shows SARS-CoV-2 Causes Transcriptional Alterations Of Endocrine-Specific Genes Leading To A Variety Of Endocrine Issues!
COVID-19 News -SARS-CoV-2 Dysregulates Endocrine Genes Nov 30, 2022 2 years, 4 months, 2 weeks, 6 days, 1 hour, 32 minutes ago
COVID-19 News: Disturbing findings from a study conducted by Italian researchers reveal that the SARS-CoV-2 coronavirus causes transcriptional alterations of endocrine-specific genes leading to a variety of endocrine issues as result of many of these genes being dysregulated while some are upregulated or downregulated compared to normal healthy settings.
The study team comprised of Italian researchers from the University of Pisa, Azienda USL Toscana nord ovest, Pisa University Hospital and University of Insubria.
Various past
COVID-19 News coverages have already covered that among Long COVID individuals, endocrine and metabolic disorders are relatively common. In spite of an increasing number of studies reporting altered blood hormones and metabolites both in the acute phase and afterwards, transcriptional alterations in endocrine organs have been barely investigated. By comparing mRNA transcript levels of genes expressed in endocrine organs of COVID-19 cases vs. controls, two major findings emerge: a) virus-containing tissues of five different endocrine organs show upregulation of ISGs. WAT represents an exception since transcripts of ISGs are activated both in virus-positive and in virus-negative COVID-19 cases; b) deregulated transcription of endocrine-specific genes is strictly organ-specific.
Obesity is an important and independent risk factor for hospitalization and mortality. It is known, in fact, that SARS-CoV-2 replicates in macrophages and adipocytes and that the adipose tissue is an important virus reservoir.
Often, obese individuals have a systemic pro-inflammatory state with abnormal production of adipokines, metabolic disorders, and hyperglycemia.
However, in COVID-19, high glucose levels associate with a remarkable increase of acute respiratory distress syndrome that leads to mechanical ventilation and high mortality.
It has been proposed that several mechanisms contribute to hyperglycemia, including systemic inflammation with insulin resistance, administration of glucocorticoids, and the viral infection of pancreatic islets.
To date, the consequences of SARS-CoV-2 infection of pancreas are controversial. While, cases of new-onset diabetes following COVID-19 have been reported and virus-infected pancreatic islets show vascular damage and fibrosis in vivo, in vitro infection by SARS-CoV-2 of human pancreatic islets is noncytopathic and produces only limited cell dysfunction.
It is already known that glucocorticoids are produced by adrenal glands and are essential to balance the immune response. I
Interestingly in critically ill COVID-19 patients, low levels of cortisol and adrenocorticotrophic hormone (ACTH) are observed.
Also, cases of central adrenal insufficiency have been reported and the genome and antigens of SARS-CoV-2 have been detected in adrenals at autopsy.
Again however, pathological changes of adrenals in COVID-19 are minimal and it is debated whether adrenal insufficiency is primary or due to impairment of the hypothalamic-pituitary-adrenal (HPA) axis. COVID-19-associated transcriptional changes of pituitary genes may play a role.
;
In the same light, the hypothalamic-pituitary-thyroid (HPT) axis may be impaired in COVID-19 possibly contributing to thyroid abnormalities. Though many patients are euthyroid, a proportion of them… especially those admitted to the intensive therapy unit tend to manifest clinical hypothyroidism with reduced levels of both thyroid stimulating hormone (TSH) and free thyroxine (T4).
A past study also reported thyrotoxicosis with risk of atrial fibrillation and thromboembolic events in about 20% of hospitalized COVID-19 patients.
In addition, controversial findings have been reported regarding sex hormones.
Although low testosterone levels associated with severe forms of COVID-19 in males, changes in sex hormones and their effects in females are not straightforward.
It has been found that SARS-CoV-2 may infect ovaries, but sex hormone levels and ovarian functions appear not to change significantly in women.
A past study observed temporary menstrual volume decrease or cycle prolongation in about 20% of women of child-bearing age that were recovering from COVID-19.
Altered blood hormone and metabolite levels during and post-COVID-19 have been extensively reported. Yet, studies of gene expression at the tissue level that can help identify the causes of endocrine dysfunctions are scarce
Typically, reports are usually limited to histopathological observations.
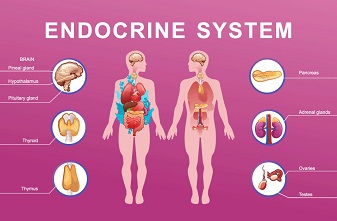
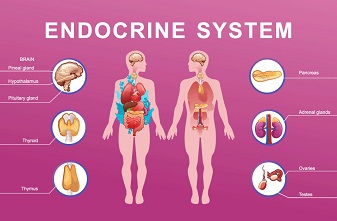
The study team evaluated the mRNA transcript levels of tissue-specific genes in five endocrine organs: adrenal gland, pancreas, ovary, thyroid, and abdominal subcutaneous white adipose tissue (WAT). Transcript levels have been compared to those of a matched control group of subjects dying abruptly of non-infectious causes.
In all, 116 autoptic specimens from 77 individuals (50 COVID-19 and 27 uninfected controls) were included. All samples were tested for SARS-CoV-2 genome. Investigated organs included adrenals, pancreas, ovary, thyroid and white adipose tissue (WAT). Transcript levels of 42 endocrine-specific and 3 IFN-stimulated genes (ISGs) were measured and compared between COVID-19 cases (virus-positive and virus-negative in tissue) and uninfected controls.
The study findings showed that ISG transcript levels were enhanced in tissues positive for SARS-CoV-2. Endocrine-specific genes (e.g., HSD3B2, INS, IAPP, TSHR, FOXE1, LEP, CRYGD) were deregulated in COVID-19 cases in an organ-specific manner. Transcription of organ-specific genes was suppressed in virus-positive specimens of ovary, pancreas and thyroid but enhanced in adrenals. In WAT of COVID-19 cases transcription of ISGs and leptin was enhanced independently of the presence of virus.
The study findings suggest that, in COVID-19, endocrine dysfunctions may arise especially when SARS-CoV-2 invades endocrine organs and that transcriptional alterations of endocrine-specific genes may contribute to endocrine manifestations.
The study findings were published on a preprint server and are currently being peer reviewed.
https://www.researchsquare.com/article/rs-2259682/v1
Consistent with previous studies, activation of ISGs genes is constantly observed in endocrine tissues infected by SARS-CoV-2. It is known that production of type I IFNs can be elicited in almost every cell type. Similarly, IFN receptors (IFNARs) are expressed on almost all cells, allowing them to acquire an antiviral state.
Interestingly, in the present study activated type I IFN responses were observed in WAT even in the absence of virus in the tissue. However, non-viral stimuli such as xenogeneic or autologous nucleic acids, activation of STING, autocrine signaling of IFNs that upregulates IRF7 may account for IFN activation.
More significantly, strong upregulation of leptin transcription has been detected in WAT of severe COVID-19 cases, independently of virus presence in the tissue.
It is known that leptin, in addition to its hormonal effects, activates lymphoid cells to produce pro-inflammatory cytokines], and high levels of leptin are associated with severe COVID-19.
Furthermore, leptin levels are also elevated in obesity, which is a major risk factor for severe COVID-19.
The study findings show that, even after adjusting for BMI, leptin transcript levels remain considerably higher in WAT of COVID-19 cases compared to controls, showing that virus infection and/or inflammatory stimuli may induce leptin transcription.
In the same light as WAT, adrenal specimens infected by SARS-CoV-2 show a substantial upregulation of HSD3B2, CYP17A1 and CYP11B1. These genes encode for enzymes that convert steroids to adrenal hormones. While the first two act in the synthesis of a wide range of steroids, CYP11B1 is specifically involved in the conversion of progesterone to cortisol.
Upregulated transcription of the above genes seems not to support a primary insufficiency of adrenals in COVID-19.
Also, an apparently controversial scenario was detected in ovaries containing SARS-CoV-2. In fact, infected ovaries exhibited downregulation of crystallin gamma D (CRYGD) and upregulation of the 5-hydroxytryptamine (serotonin) receptor 1A (HTR1A) gene.
Crystallin gamma D has a very similar sequence and structure to that of crystallin beta, but it is monomeric.
Although there are no clear attributed functions of gamma-crystallin in ovaries, beta-crystallin does influence female fertility by regulating apoptosis in granulosa cells and follicular atresia.
Thus, the downregulation of CRYGD may be consistent with alterations of the menstrual cycle observed in women recovering from COVID-19.
Also, the enhanced expression of serotonin receptor 1A is in line with decreased serotonin serum levels observed in severe COVID-19 cases. Similar to what found in humans, in mice the Zika virus also targets the ovaries inducing a type I IFN response that is associated with disordered steroidogenesis.
In the case of the thyroid gland, alterations of gene transcription were selectively observed when SARS-CoV-2 was present in the tissue. Changes affected factors associated with thyroid dysfunction.
It was found that the transcription of ZNF804B and FOXE1 was downregulated; ZNF804B is possibly associated with antiviral defense, while FOXE1 promotes the expression of multiple thyroid-specific genes, including those encoding for thyroglobulin, thyroid peroxidase, thyroid dual oxidase 2, pendrin and other transporters.
It was also found that the TSHR gene was downregulated. Since serum TSH levels are generally low in mild to severe forms of COVID-19, low levels of the TSH receptor indicate a possible impairment of the HPT axis.
In a scenario of suppressed function, the enhanced expression of thyroid peroxidase may appear not justified. However, non-endocrine regulatory mechanisms may be operative during microbial stress responses. Indeed, thyroid peroxidase is a major autoantigen in thyroid autoimmunity and a key player against oxidative stress.
The exocrine and endocrine pancreatic tissue deserves a separate discussion.
In COVID-19 cases, the pancreas is the only tissue for which alterations of gene transcription are seen in the absence of activated IFN responses and independently of the viral presence in the tissue.
Also, the expression of pancreatic lipase-related protein 1 (PNLIPRP1) was enhanced. Differently from its paralogs (pancreatic triacylglycerol lipase and PNLIPRP2), PNLIPRP1 lacks lipolytic activity and also inhibits pancreatic lipase; thus, enhancement of a lipase inhibitor may be part of a defensive response.
In addition, suppression of lipid catabolism may be linked to a switch of infected cells to glycolytic metabolism.
Importantly, the study findings show the downregulation of two beta cell genes that code for insulin (INS) and islet amyloid polypeptide (IAPP).
Both these hormones are crucial in the regulation of blood glucose levels, and are frequently downregulated in diabetes.
The study findings support a potential failure of beta cells in COVID-19 and reminds that stress associated with a reduction of intracellular proinsulin may activate inflammatory pathways in beta-cells.
It was also found unexpectedly that somatostatin (SST) mRNA transcripts were downregulated only in virus-negative pancreas specimens. Somatostatin is produced by pancreatic delta cells and regulates pituitary growth hormone, thyroid stimulating hormone, and most hormones of the gastrointestinal tract.
Contextualization of somatostatin downregulation in COVID-19 needs further attention.
The study findings showed the transcriptional alterations in endocrine organs of individuals who died because of COVID-19 are tissue-specific. In most organs, significant changes were observed only when the SARS-CoV-2 genome was present in tissue.
While infected ovary and thyroid showed downregulation of tissue-specific genes, in adrenals transcription of endocrine genes was enhanced, possibly as part of the stress response.
In beta cells hormone genes were suppressed independently of the presence of virus in the tissue. This is reminiscent of type 1 diabetes where beta cell functions are inhibited in an inflammatory context.
In WAT, the enhanced transcription of functional genes is independent of virus presence in tissue and may be linked to the inflammatory context.
The study findings provide evidence that endocrine dysfunction may arise in COVID-19, especially when the virus invades endocrine organs. Clinicians should be aware that endocrine manifestations in the acute phase of COVID-19 and in the post-COVID syndrome may derive from transcriptional changes of endocrine-specific genes.
For the latest
COVID-19 News, keep on logging to Thailand Medical News.