COVID-19 News: Malaysian Researchers Warn That SARS-CoV-2 Infections Can Cause Myelin Oligodendrocyte Glycoprotein Antibody-Associated Optic Neuritis
Nikhil Prasad Fact checked by:Thailand Medical New Team Oct 28, 2023 1 year, 11 months, 2 weeks, 5 days, 27 minutes ago
COVID-19 News: The COVID-19 pandemic has undeniably transformed the way we perceive health, leading to unprecedented research efforts and discoveries in the field of medicine. As the virus's impact reaches far beyond the respiratory system, its consequences on various organs have been unveiled, and the eye, surprisingly, is no exception. In a recent report from the Department of Ophthalmology at the Faculty of Medicine, Universiti Kebangsaan Malaysia in Kuala Lumpur, Malaysian researchers warn that SARS-CoV-2 infections can cause Myelin Oligodendrocyte Glycoprotein Antibody-Associated Optic Neuritis (MOG ON). This case report covered in this
COVID-19 News report underscores the importance of understanding the complex and diverse manifestations of COVID-19 and its implications for the optic nerve.
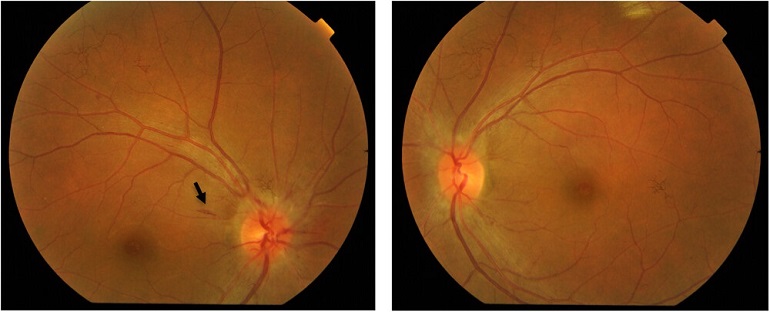
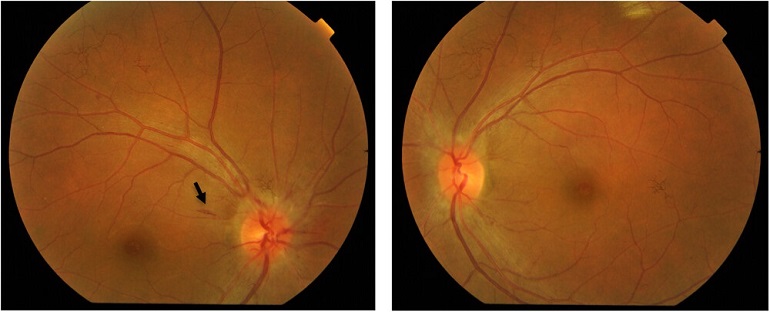 Bilateral optic disc swelling seen at presentation. Circumferential halo of disc edema and splinter haemorrhage (black arrow) temporally (black arrow) was seen on the right eye and C-shaped halo of disc edema was seen sparing the temporal disc margin on left eye.
Case Report
Bilateral optic disc swelling seen at presentation. Circumferential halo of disc edema and splinter haemorrhage (black arrow) temporally (black arrow) was seen on the right eye and C-shaped halo of disc edema was seen sparing the temporal disc margin on left eye.
Case Report
The case at hand involves a 36-year-old Malay gentleman with a history of hypertension. He presented with a bilateral, progressive blurring of vision over a week, accompanied by retrobulbar pain. Remarkably, there were no other neurological symptoms present. One week prior, he had experienced fever and had tested positive for COVID-19. It's noteworthy that he had received the COVID-19 booster vaccine a month before the onset of his illness. His COVID-19 infection was categorized as mild, and he self-quarantined at home.
Upon examination, his vision was seriously compromised. His right eye could only perceive hand motions, and his left eye was limited to 6/18 vision. Furthermore, a relative afferent pupillary defect (RAPD) was detected in his right eye, along with abnormal optic nerve function tests. Remarkably, the anterior segments of his eyes appeared normal. However, the fundus examination revealed bilateral optic disc swelling. Subsequent MRI investigations displayed multifocal hyperintense subcortical white matter lesions, with the optic nerves appearing normal and showing no enhancement. These observations, along with the patient's positive serum MOG antibody, confirmed the diagnosis of MOG ON.
Treatment and Outcome
To combat the MOG ON, the patient was administered intravenous methylprednisolone followed by oral prednisolone, adhering to the Optic Neuritis Treatment Trial (ONTT) protocol. This treatment regimen led to a marked improvement in the patient's vision and ocular symptoms, along with the resolution of retrobulbar pain and optic disc swelling. The patient was then prescribed oral prednisolone, with a tapering dosage, and azathioprine was added to his treatment plan. At one month, the patient's condition remained stable, with no signs of recurrence.
Understanding MOG Antibody-Associated Optic Neuritis
MOG ON is a rare autoimmune condition that primarily affects the optic nerve and is chara
cterized by the presence of myelin oligodendrocyte glycoprotein (MOG) antibodies in the patient's serum. Traditionally, MOG ON is known to present with severe bilateral sequential visual loss accompanied by optic disc edema, retinal venous congestion, optic perineuritis, and myelitis. However, the case discussed in this report highlights a somewhat milder presentation of MOG ON associated with COVID-19.
The pathophysiology of MOG ON remains incompletely understood, but it is believed that MOG antibodies target MOG receptors on oligodendrocytes. These antibodies can circulate freely in the body, and in the presence of inflammation or infection, they can access the central nervous system. This access then triggers a cascade of immune-mediated reactions, leading to various neurological manifestations, including encephalitis, transverse myelitis, optic neuritis, cranial nerve palsy, nystagmus, visual field defects, and other autoimmune diseases like Kawasaki disease, Miller Fisher syndrome, and Guillain–Barré syndrome.
Instances of MOG ON linked to COVID-19 infection have been reported globally, showcasing the complexity of the virus's impact on the nervous system. Some cases involve both optic neuritis and myelitis, while others manifest as unilateral optic neuritis. Notably, a common thread among these cases is the promising response to high-dose intravenous corticosteroids, which is a hallmark of MOG ON.
COVID-19 and MOG ON
This case report not only sheds light on the unique presentation of MOG ON in the context of a COVID-19 infection but also raises important questions about the interplay between the virus, vaccination, and autoimmune responses. Some key observations from this case and others in the literature are as follows:
-Mild COVID-19 Manifestation: In some cases, neurological symptoms like optic neuritis have been observed in individuals with mild COVID-19 infections. This underscores the virus's capacity to affect the nervous system across the spectrum of disease severity.
-MOG Antibodies: The presence of MOG antibodies in patients who have experienced COVID-19 suggests a possible link between the virus and MOG ON. This may be related to the virus triggering autoimmune responses that lead to the production of MOG antibodies.
-Recurrence Rates: Interestingly, MOG ON associated with COVID-19 has shown a lower recurrence rate compared to classical MOG-related optic neuritis. This is a significant departure from the typical pattern of MOG ON, which tends to be recurrent.
-Vaccination and Autoimmune Responses: There is a possibility that COVID-19 vaccination may have adverse effects, including autoimmune responses. In this case, the patient had received a booster vaccine two months prior to developing MOG ON, suggesting a potential connection between the vaccine and autoimmune reactions.
Conclusion
The case of MOG ON associated with COVID-19 is a reminder of the virus's complex and diverse impact on the human body. While much remains to be understood about the pathogenesis of MOG-related CNS inflammation following COVID-19 infections, the promising response to high-dose corticosteroid therapy is a hopeful sign for patients who may experience this condition.
As the world continues to grapple with the ongoing COVID-19 pandemic, research like this case report is vital in expanding our knowledge of the virus's effects and in guiding the development of effective treatments. It serves as a testament to the importance of ongoing research and vigilance in monitoring the health of individuals affected by COVID-19. Furthermore, it underscores the necessity of thorough investigations into the potential adverse effects of vaccinations and the role they might play in autoimmune responses.
In the ever-evolving landscape of COVID-19, researchers and healthcare professionals must remain vigilant, open to new discoveries, and prepared to adapt to the unpredictable nature of the virus. Cases like the one described here are a stark reminder of the importance of interdisciplinary collaboration and continued research efforts in our global fight against COVID-19.
The case report was published in the peer reviewed journal: Immunity, Inflammation and Disease. (Wiley)
https://onlinelibrary.wiley.com/doi/10.1002/iid3.1051
For the latest
COVID-19 News, keep on logging to Thailand Medical News.