COVID-19 News: Researchers Warn That SARS-CoV-2 Can Trigger And Also Aggravate Fibromyalgia Syndrome!
COVID-19 News -SARS-CoV-2 Triggers Fibromyalgia Mar 01, 2023 2 years, 1 month, 2 weeks, 5 days, 4 hours, 22 minutes ago
COVID-19 News: Researchers from the Federal University of Santa Maria-Brazil are warning that SARS-CoV-02 infections can trigger fibromyalgia (FM) syndrome and also aggravate conditions in those already afflicted with fibromyalgia!
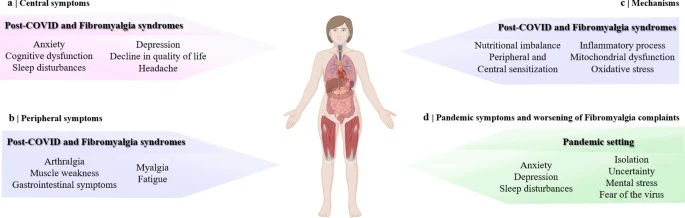
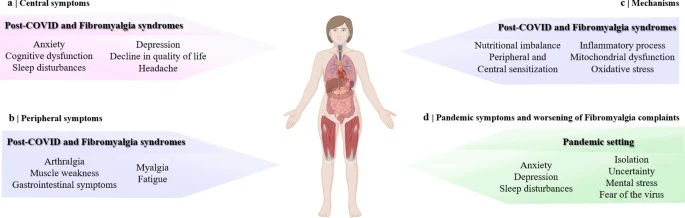 Graphical Abstract
Graphical Abstract
Fibromyalgia (FM) is a disorder characterized by widespread musculoskeletal pain accompanied by fatigue, sleep, memory and mood issues. Researchers believe that fibromyalgia amplifies painful sensations by affecting the way your brain and spinal cord process painful and nonpainful signals.
Though it’s a complex disease with an uncertain aetiology and intricate pathophysiology, some other factors have been weakly associated with the onset of fibromyalgia, but more research is needed to see if they are real. These possible risk factors include:
-Sex. Women are twice as likely to have fibromyalgia as men.
-Stressful or traumatic events, such as car accidents, post-traumatic stress disorder (PTSD)
-Repetitive injuries. Injury from repetitive stress on a joint, such as frequent knee bending.
-Illness (such as viral infections)
-Family history
-Obesity
https://www.cdc.gov/arthritis/basics/fibromyalgia.htm
Already it is known that the SARS-CoV-2 virus may affect central and peripheral nervous systems, leading to musculoskeletal, neurological, and psychological disturbances. These symptoms might persist at least 12 months beyond the recovery, often referred to as post-COVID syndrome, which resembles FM syndrome.
Past
COVID-19 News coverages have already indicated that many Long COVDI individuals are also manifesting fibromyalgia.
https://www.thailandmedical.news/news/breaking-study-warns-that-fibrocovid-or-fibromyalgia-as-a-result-of-a-sars-cov-2-variant-infection-is-now-a-growing-occurrence-of-long-covid
SARS-CoV-2 Infections Could Trigger Fibromyalgia
Numerous similarities between post-COVID syndrome and the FM syndrome raise the hypothesis that SARS-CoV-2 infection could trigger the development of FM once potential environmental factors generate it.
https://pubmed.ncbi.nlm.nih.gov/27189527/
t;
https://pubmed.ncbi.nlm.nih.gov/33024295/
Certain viral infections have been linked to the development of FM, including infection induced by the hepatitis C virus, human immunodeficiency virus (HIV), parvovirus, or Epstein–Barr virus.
https://pubmed.ncbi.nlm.nih.gov/18706528/
The findings that such infectious agents are associated with FM syndrome suggests that abnormal host response to infection may be implicated.
https://pubmed.ncbi.nlm.nih.gov/34175230/
Hence, the hypothesis that SARS-CoV-2 and its sequelae might play a role in the development of FM is encouraged.
Clinical features of the FM syndrome, such as musculoskeletal pain, fatigue, sleep impairment, depression, and anxiety have been reported in one-third of patients with symptoms of the post-COVID syndrome.
Web-based research uncovered more than 600 patients that developed post-COVID syndrome. Of them, about 30% of patients met the 2011 American College of Rheumatology (ACR) criteria for diagnosis of FM at a mean of 6 months after their recovery from COVID-19. Therefore, they were referred to as post-COVID FM.
https://pubmed.ncbi.nlm.nih.gov/34426540/
Interestingly, the comorbidity of obesity and male gender also seem to be risk factors for developing the post-COVID FM-like syndrome in this subgroup of interviewed patients.
The researchers in that previous study have suggested that patients who developed severe COVID-19 (with hospital admission and oxygen therapy need) are more suggestive of developing a post-COVID FM-like syndrome.
However, in another study, 56.7% of patients (17/30) who showed mild and moderate symptoms during COVID-19 were positive for FM-like symptoms 6 months after the infection. Thus, the severity of the symptoms during the disease course seems not to be an essential factor for developing a post-COVID FM-like syndrome.
https://pubmed.ncbi.nlm.nih.gov/34245450/
Significantly, one case report published in April 2021 also demonstrated the strong relationship between FM symptoms and post-COVID syndrome.
https://www.openaccessjournals.com/articles/coronavirus-disease-2019-covid19-an-emerging-trigger-for-primary-fibromyalgia-syndrome-a-tale-of-three-cases-postcovid19-14615.html
It was reported that three female patients with no previous history of FM or any other rheumatic disease complained of persistent symptoms after recovery from COVID-19, such as generalized musculoskeletal pain, allodynia, fatigue, anxiety, depression, paraesthesia, and non-restorative sleep. General examination and several laboratory investigations, including an autoimmune profile and radiological investigation, were all normal.
All the women met the 2010 ACR criteria for a diagnosis of FM. The standard clinical treatments of FM, including non-pharmacological and pharmacological management, were prescribed to them, such as physical exercise and therapies approved by FDA, including duloxetine ((serotonin and norepinephrine reuptake inhibitor (SNRI)) and gabapentin (gabapentinoid).
All women reported improved well-being and mood after the onset of treatment, which contributed to confirming the diagnosis of a post-COVID FM-like syndrome.
In another case report involved a woman diagnosed with COVID-19 without a history of any previous painful condition but with some associated comorbidities.
https://pubmed.ncbi.nlm.nih.gov/32779108/
The female patient presented with pain symptoms very similar to the complaints reported by patients with FM, which included: (i) constant neck and back pain (resembling generalized pain), (ii) and a burning quality (resembling a neuropathic-like FM pain), which was (iii) exacerbated by light touch and heat (resembling mechanical and thermal hypersensitivity). This patient presented with bilateral and generalized pain, which was not a pattern for viral neuropathic pain. Furthermore, the onset of the pain coincided with her SARS-CoV-2 infection, and there was no other likely explanation for the symptoms. Sleep problems, which are observed in many patients with FM, were also reported. The patient's treatment with acetaminophen, non-steroidal anti-inflammatory drugs (NSAIDs), and opioids did not alleviate her pain.
This made the study team to hypothesize that this patient was going through a post-COVID FM-like syndrome once these usual treatment approaches are ineffective for patients with FM. On the other hand, gabapentinoids, a class of drugs recommended for the treatment of FM, attenuated the painful hypersensitivity and improved the sleep quality of this patient.
Research published so far speculate that the development of FM might be occasioned in a subgroup of patients after SARS-CoV-2 infection. However, it is currently unknown what factors contribute to it.
However potential processes have been suggested for the pathophysiology of post-COVID syndrome. These processes might also be linked to the development of FM syndrome after the viral infection. Substantial mechanisms that may contribute to the trigger of an FM-like syndrome after COVID-19 are:
-pathophysiologic changes caused by SARS-CoV-2 itself, mainly neuropsychiatric sequelae such as chronic malaise, diffuse myalgia, depressive and anxiety symptoms, non-restorative sleep, and cognitive impairment.
-SARS-CoV-2 cell-to-cell inflammatory mechanisms (ie, cytokine storms) which might provoke hyperexcitability of PNS and CNS.
-sequelae of post-critical illness are indirect processes responsible for worsening the physical, cognitive, and psychiatric domains after COVID-19. They can be caused by posttraumatic stress disorder, prolonged bed rest, ICU admission, and the necessity of sedation and ventilation.
The co-existence of comorbidities or immunosuppressive diseases is a known factor for anticipating or developing chronic pain and increasing severity and mortality related to COVID-19. Thus, it can also be suggested that the presence of these parameters might support the advancement of FM-like symptoms after COVID-19.
The early recognition of the development of an FM-like syndrome after COVID-19 could lead to prompt and targeted treatment and, thus, mitigate the potential impact of chronic pain on health and the social environment.
Existing Fibromyalgia Could Be Aggravated By SARS-CoV-2 Infection.
It has also been proposed that individuals living with FM are an extremely vulnerable population in the setting of COVID-19.
https://pubmed.ncbi.nlm.nih.gov/33204998/
It has been demonstrated that patients with FM are subject to more significant mental stress and anxiety during COVID-19. Thus, these patients have exacerbated symptoms of pain, fatigue, and sleep quality compared to control patients (without FM) with COVID-19. Therefore, the SARS-CoV-2 infection may be an essential factor in exacerbating the symptoms of FM patients.
https://pesquisa.bvsalud.org/global-literature-on-novel-coronavirus-2019-ncov/resource/fr/covidwho-924960
It should be noted that acute symptoms of COVID-19 can persist in COVID-19 survivors after their recovery.
https://pubmed.ncbi.nlm.nih.gov/32458242/
Hence, it is unclear if the exacerbation of FM symptoms returns to normal after patients with FM have recovered from COVID-19.
Also, it has been shown that patients suffering from pre-existing musculoskeletal pain conditions before COVID-19 seem to experience increased intensity, extension, or frequency of their symptoms for at least the first seven months after infection.
https://pubmed.ncbi.nlm.nih.gov/34561390/
https://pubmed.ncbi.nlm.nih.gov/33863864/
Hence, it can be speculated that the enhanced FM symptoms in post-COVID situations can also last for an extended time.
Typically, individuals with FM are at increased risk of mood disorders, even in non-pandemic situations.
During the COVID-19 pandemic, the social and economic environments where individuals live and work suffered changes. Thus, the COVID-19 pandemic prompted feelings of isolation, uncertainty, depression, mental stress, generalized anxiety, and fear of the virus, mainly in vulnerable subgroups.
Some studies have even revealed that fear and anxiety levels during the COVID-19 pandemic in patients with FM were higher than in control patients (without FM).
https://pubmed.ncbi.nlm.nih.gov/34193303/
Another research reported that 67% of 32 patients with FM had their general health status (well-being) worsened during the lockdown imposed by the COVID-19 pandemic.
https://academic.oup.com/rheumatology/article/60/1/465/5981977
These feelings seem to be associated with the severity of painful symptoms of FM. The lack of social interactions may also play an essential role in modulating pain and dealing with chronic pain. Furthermore, patients with FM appear to be more susceptible to mood disorders than patients with other rheumatic diseases in the settings imposed by the COVID-19 pandemic, reinforcing the need to care for patients suffering from FM.
https://pubmed.ncbi.nlm.nih.gov/34161226/
The study findings so far indicate that FM symptoms might be exacerbated during COVID-19, at least in a subset of patients, and it can persist for months after recovery.
https://pesquisa.bvsalud.org/global-literature-on-novel-coronavirus-2019-ncov/resource/fr/covidwho-924960
https://pubmed.ncbi.nlm.nih.gov/33753937/
Considering the global scale of this pandemic, it is apparent that the healthcare needs for patients with sequelae of COVID-19 will continue to increase for the foreseeable future. Current evidence raises several interesting questions about whether FM syndrome, a chronic pain condition, might be triggered or potentiated by COVID-19.
The study findings were published in the peer reviewed journal: Inflammopharmacology.
https://link.springer.com/article/10.1007/s10787-023-01160-w
For the latest
COVID-19 News, keep on logging to Thailand Medical News.