COVID-19 News: Russian Study Finds That SARS-CoV-2 Infections Can Cause Cholinergic Deficiency Leading To Various Serious Health Conditions!
COVID-19 News - SARS-CoV-2 Disrupts Signaling In Acetylcholine System Feb 25, 2023 2 years, 9 months, 3 weeks, 3 days, 23 hours, 39 minutes ago
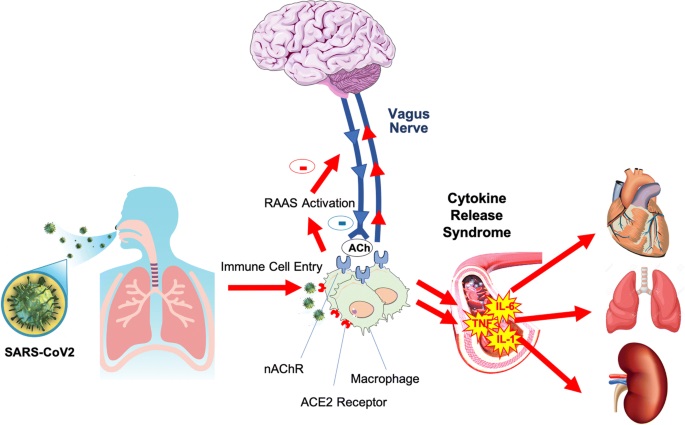
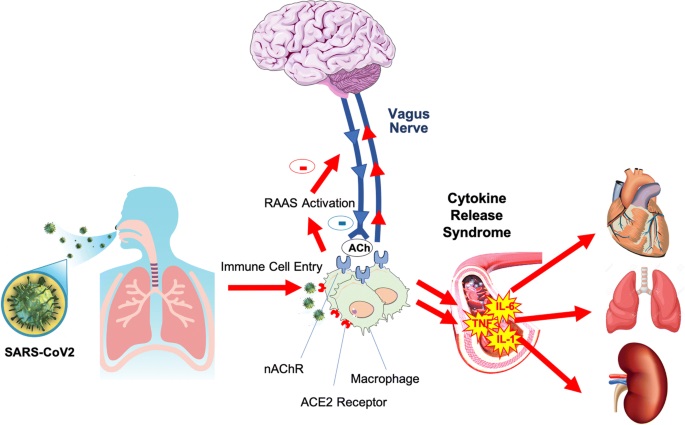
COVID-19 News: Researchers from Maikop State Technological University, Republic of Adygeya-Russia and Adyghe State University-Russia in a new study have discovered that SARS-CoV-2 infections can cause disruptions in the signaling of the acetylcholine system (AChS) in the human host, causing cholinergic deficiency that can lead to various serious symptoms and health conditions arising especially cardiovascular issues!
To date, several mechanisms of viral invasion of the central nervous system (CNS) have been proposed, one of which is both direct penetration of the virus through afferent nerve fibers and damage to the endothelium of cerebral vessels.
It has been proven that the SARS-CoV-2 virus affects pathologically not only the human cardiorespiratory system but is also associated with a wide range of neurological diseases, cerebrovascular accidents, and neuromuscular pathologies.
However, the observed post-COVID symptom complex in patients, manifested in the form of headache, “fog in the head,” high temperature, muscle weakness, lowering blood pressure, made the study team to think about the pathophysiological mechanisms that contribute to the development of this clinical picture.
The study team says that one possible explanation is a disruption in the signaling of the acetylcholine system (AChS) in the body. Viral invasions, and in particular COVID-19, can negatively affect the work of the AChS, disrupting its coordination activities.
The key objective of this meta-analysis study was to analyze the information and substantiate the possible mechanisms for the occurrence of post-COVID syndrome in people who have had COVID-19 from the standpoint of AChS dysfunctions.
According to the study team, the AChS works as a powerful cooperative apparatus, having both multiple information inputs from numerous brain structures and outputs. To date, it is known that a large number of acetylcholine (ACh) neurons, sending numerous processes to the cortex and subcortical formations, are located in the brain, especially in the forebrain and brainstem.
The presence of the AChS in the brain is an important component of the proper development of the brain and its functions, which provides the synaptic plasticity necessary for the formation of memory and learning. AChS plays a special role in the hippocampus and prefrontal cortex, which are responsible for these functions, where a huge number of ACh synapses and corresponding processes have been found.
The activation of ACh receptors (AChRs) in these regions of the brain increases the generation of theta and gamma rhythms. These rhythms are responsible for cognitive functions.
It has been proven that not only memory capacity and intelligence play a role in the learning process, but also attention.
The AChS also plays an important role in various physiological and pathophysiological processes, including the regulation of the muscular system, immune and inflammatory reactions, wound healing, the development of cardiovascular, respiratory, and other diseases.
The use of synaptic transmission through a chemical synapse is the main way information is transmitted in the nervous system. The neuromuscular synapse and central synapse include the presynaptic region of the nerve ending, the synaptic cleft, a
nd the postsynaptic region (motor end plate)
The study finding showed a number of pathophysiological changes in acetylcholine system in COVID-19 survivors
.
The study findings were published in the peer reviewed Chinese Journal of Physiology.
https://www.cjphysiology.org/article.asp?issn=0304-4920;year=2023;volume=66;issue=1;spage=1;epage=13;aulast=Lysenkov
To date, no
COVID-19 News coverages have covered this topic about SARS-CoV-2 infections causing cholinergic deficiency and it has been a overlooked area.
It should be noted that even after recovery, people who have had COVID-19 experience headache, brain fog, periodic fever, muscle weakness, and memory impairment might last for a long time. One of the possible causes for the development of this symptomatology, according to the study team is a disorder of the AChS in the body. The release of pro-inflammatory cytokines IL-1, IL-2, IL-6, TNF-α, γ stimulates the production of nitric oxide, and activation of calcium channels, which leads to an increase in ACh exocytosis.
A high concentration of nitric oxide in the synaptic space leads to the inhibition of AChE, which increases the residence time of ACh in the synaptic cleft. On the other hand, the occurrence of a “cytokine storm” activates the synthesis of all forms of nitric oxidesynthase (NOS), inducing the production of a large amount of NO, which can be oxidized to the toxic product – peroxynitrite. The latter reacts with lipids of pre-synaptic and postsynaptic membranes and disrupts the processes of endo- and exocytosis of ACh.
In addition, oxidation and denaturation of protein-lipid complexes of ACh, Na+, Ca2+ channels occur. It should also be noted that a disorder of calcium metabolism leads to an increase in its concentration and a significant change in the potentiation time, and, as a result, depletion of ATP reserves, as well as disruption of the actin-myosin coupling and relaxation. Increasing the concentration of calcium leads to disruption of the mitochondria and the accumulation of products of reactive oxygen species (ROS).
Acetylcholine System Disorders and Effects on the Cardiovascular System
It has been found that many post-COVID patients often complain about pathologies of the cardiovascular system: cardiac arrhythmias and orthostatic collapses.
It is noted in many studies, that 1/3 or more of those with COVID have a lesion of the cardiovascular system. However, the study team notes that damage to the cardiovascular system in most cases is not directly related to viral invasion, and the nature of the pathologies is not entirely clear.
The researchers believe that after suffering from COVID-19 disease, disturbances in the autonomic nervous system can significantly affect the functions of the cardiovascular system, expressed in the inadequacy of orthostatic, due to impaired sympathetic control of tone, vessels during the redistribution of blood volume under the influence of gravity.
The innervation of resistive vessels is provided through the sympathetic ganglia, in which ACh acts as a mediator. The loss of sympathetic tone is probably due to a deterioration of neuromuscular transmission in adrenergic synapses of vascular smooth muscles.
Inflammation of the endothelium (systemic endotheliitis) in COVID infection causes energy processes to be disrupted in all underlying subendothelial areas, including vascular muscles and synapses.
Despite the strong influence of the central sections of the CNS on the work of the heart through the parasympathetic and sympathetic sections, it is necessary to take into account the fact that there are intracardiac reflex arcs, which include Dogel cells (1, 2, 3 orders) with the mediator ACh. These reflexes normally provide a rapid restructuring of the heart, after which the mechanisms of systemic regulation are activated through the vasomotor and cardioinhibitory centers.
Loss of control from the vagus nerve (its afferent and efferent links) may be accompanied by attacks of tachycardia and the appearance of ectopic foci in the myocardium.
Similar reactions were noted in the elderly. It has been shown that with age the efficiency of cardiovagal baroreceptor regulation decreases due to modification of the receptors of the aortic arch, carotid sinus, cardiopulmonary, and other reflexogenic zones. Under physiological conditions, lowering blood pressure (BP) includes baroreflex regulation of cardiac activity and blood vessels. It consists of a narrowing of resistive vessels, tachycardia, and an increase in BP, as well as due to the release of adrenaline from the adrenal medulla in response to a decrease in BP. However, it can be assumed that reflex responses in some cases after exposure to the virus will be inadequate and delayed in some patients due to a malfunction of the ACh synapse that innervates this area.
Study Conclusions:
The study findings showed that AChS failure, caused by hyperproduction of pro-inflammatory interleukins and nitric oxide, is formed in conditions of COVID infection. The latter, through stimulation of MNDA receptors and calcium channels, stimulates an active release of ACh into synapses, with a sharp inhibition of acetylcholinesterase activity, prolonged activation of Na channels, followed by a deterioration of signal transmission in the neuromuscular, nerve and neuroimmune synapse. An important element is the effect of the COVID-19 virus to form viroporins, their own calcium channels, through which the virus enters the cell and replicates in it. At the same time, the level of plasma calcium decreases, but the mechanism of hypocalcemia remains debatable.
Hyperproduction of nitric oxide is accompanied by the formation of a powerful oxidizing agent, peroxynitrite, which causes modification of the protein and lipid components of the AChR, Ca2+, and Na channels, which even more disrupts the transmission of signals from the presynaptic to the postsynaptic membrane.
Clinically, this is manifested by severe muscle fatigue in patients, the development of a “cytokine storm” and various neuropsychiatric disorders. The modification of AChR protein-lipid compounds, protein-lipid formations of Na+-, Ca2+-channels is accompanied by an immune response to self-antigens.
Cholinergic deficiency develops after a period of activation of the release of ACh into the synapse, especially during the cytokine storm at the stage of the process subsiding. An autoimmune chronic process is formed with periodic manifestation of one or another syndrome (arthritis, artalgia, myalgia, myasthenia gravis, diabetes mellitus, synovitis, and Guillain–Barré syndrome). The phasic nature of the functioning of the acetylcholine system in viral infection dictates the need for a differentiated approach to treatment at different stages of the inflammatory response.
The study team proposes that to improve the function of ACh-synapses in the post-COVID period, the use of anticholinesterase drugs is pathogenetically justified.
For the latest
COVID-19 News, keep on logging to Thailand Medical News.