COVID-19 News: SARS-CoV-2 Spike Protein Causes And Accelerates Systemic Sclerosis By Upregulating Inflammatory Cytokines, Th17 Cells And Fibrosis!
Nikhil Prasad Fact checked by:Thailand Medical News Team Dec 23, 2023 1 year, 3 months, 3 weeks, 3 days, 2 hours, 18 minutes ago
COVID-19 News: The seismic impact of the COVID-19 pandemic, orchestrated by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), extends far beyond the realms of respiratory distress, delving into the intricate landscapes of autoimmune diseases. Among these, systemic sclerosis (SSc) has emerged as a noteworthy player, sharing symptomatic parallels with COVID-19, including immune dysfunction, inflammation, and coagulopathy. The unfolding research at The Catholic University of Korea covered in this
COVID-19 News report, delves into the subtle connections between COVID-19 and SSc, revealing a potential accelerant in the form of the SARS-CoV-2 spike protein.
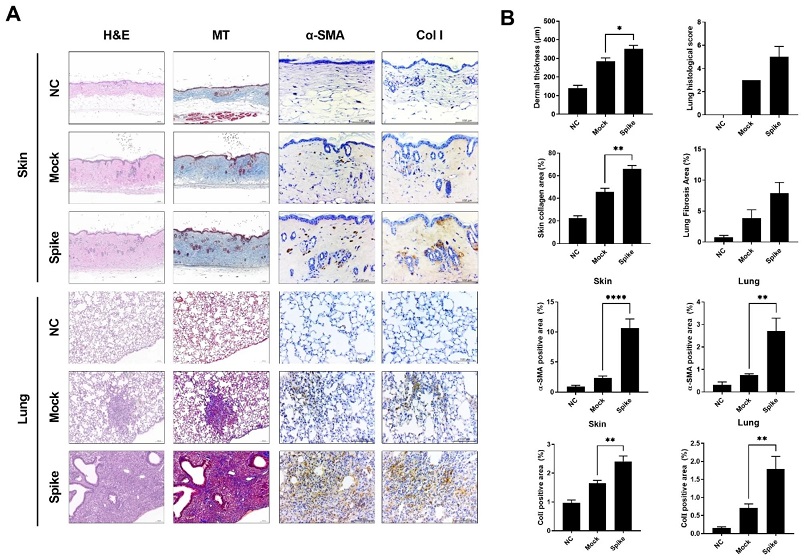
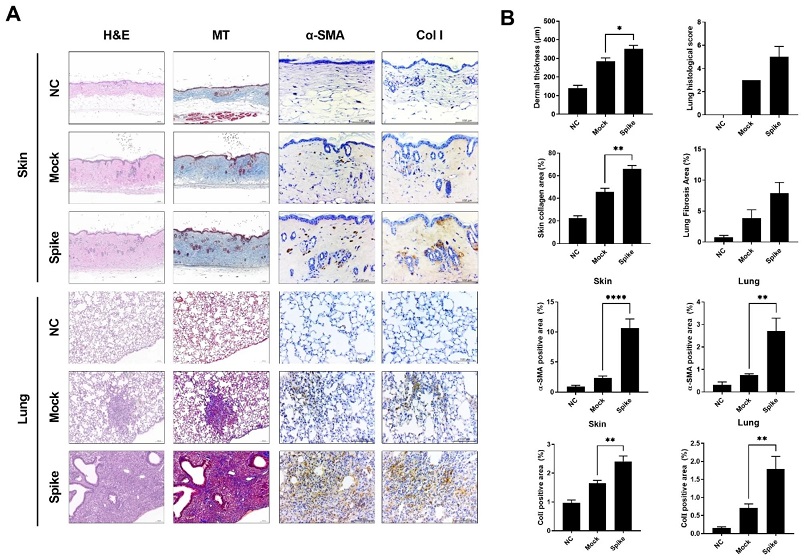 Induction of fibrosis in skin and lung tissues in BLM-Induced SSc mice following injection of pcDNA3.1-SARS2-Spike and pLEX307-ACE2-puro (n = 5). (a) Histological analysis of skin and lung tissues isolated from sacrificed SSc mouse models at 5 weeks post-injection, stained with hematoxylin & eosin, Masson’s trichrome, and subjected to immunohistochemistry analysis for α-SMA and collagen type I. (b) Graph representing skin dermal thickness, lung histological score, collagen area, α-SMA, and collagen type I positive area in skin and lung tissues
Systemic Sclerosis and COVID-19: A Confluence of Challenges
Induction of fibrosis in skin and lung tissues in BLM-Induced SSc mice following injection of pcDNA3.1-SARS2-Spike and pLEX307-ACE2-puro (n = 5). (a) Histological analysis of skin and lung tissues isolated from sacrificed SSc mouse models at 5 weeks post-injection, stained with hematoxylin & eosin, Masson’s trichrome, and subjected to immunohistochemistry analysis for α-SMA and collagen type I. (b) Graph representing skin dermal thickness, lung histological score, collagen area, α-SMA, and collagen type I positive area in skin and lung tissues
Systemic Sclerosis and COVID-19: A Confluence of Challenges
Systemic sclerosis, also known as scleroderma, stands as a multifaceted autoimmune connective tissue disease marked by extensive vasculopathy, immune system dysregulation, and pathological fibrosis affecting both the skin and internal organs. As COVID-19 ravages the globe, its primary target being the respiratory tract, the overlap of symptoms and risk factors with autoimmune conditions has ignited a quest for understanding the relationship between COVID-19 and diseases like SSc.
A Meta-Analysis Lens: Autoimmune Diseases and COVID-19 Prevalence
Extensive meta-analyses have drawn attention to the heightened vulnerability of patients with autoimmune diseases, such as rheumatic diseases and inflammatory bowel disease, to COVID-19 infection. The compromised immune systems of individuals undergoing immunosuppressive treatments render them more susceptible to severe clinical manifestations of COVID-19. The meta-analysis encompassing 62 observational studies highlights a higher prevalence of COVID-19 in autoimmune disease cohorts compared to the general population.
Pulmonary Fibrosis in SSc: A Lethal Complication
Pulmonary fibrosis, often synonymous with interstitial lung disease (ILD), stands as a critical pulmonary manifestation in SSc patients, emerging as a leading cause of SSc-related mortality. The absence of a targeted and fully effective treatment for SSc-related ILD poses a significant challenge for clinicians. With COVID-19 predominantly affecting the respiratory system and individuals on immunosuppressive regimens being predisposed to infections, the intersection of these two conditions amplifies the complexity of patient management.
Clinical Insights: Unveiling th
e Impact of COVID-19 on SSc
Insights from clinical observations, particularly from Brazilian SSc patients, provide a nuanced perspective on the consequences of COVID-19 infection. Notably, those with moderate-to-severe COVID-19 exhibited a higher incidence of ILD, pulmonary arterial hypertension (PAH), and cardiac involvement.
Strikingly, reports have surfaced of individuals devoid of any SSc history developing clinical symptoms indicative of the disease after recovering from COVID-19. Case studies narrate instances where individuals, previously in good health, manifested symptoms akin to SSc after COVID-19 infection. This study seeks to explore the intricacies of how SARS-CoV-2 might impact the progression of SSc through a meticulous investigation utilizing a bleomycin-induced SSc mouse model.
Research Findings: SARS-CoV-2 Spike Protein's Role Unveiled
The study conducted at The Catholic University of Korea presents a compelling narrative of the intricate dance between the SARS-CoV-2 spike protein and the development of systemic sclerosis. Employing human embryonic kidney cells (HEK293) in vitro, researchers observed that the spike protein induced elevated levels of fibrosis-related proteins, hinting at its potential role as a mediator in promoting fibrosis.
Moving to in vivo experiments using a bleomycin-induced SSc mouse model, exposure to the SARS-CoV-2 spike protein resulted in a cascade of effects. Increased skin thickness, elevated levels of autoantibodies, thrombotic factors, and inflammatory cytokines painted a picture of accelerated disease progression.
The study shed light on the heightened expression of the proinflammatory cytokine IL-17 in the skin, lungs, and blood of SSc mice subjected to the spike protein. Moreover, tissue fibrosis and inflammatory cytokine levels in the skin and lungs exhibited a marked escalation in the presence of the protein.
Understanding Mechanisms: The Spike Protein's Impact on Immune Response
The research team hypothesized that the SARS-CoV-2 spike protein might serve as a catalyst, exacerbating the immune response and fibrosis in SSc. In-depth analyses revealed that the protein induced fibrosis in HEK293 cells and aggravated SSc in the mouse model. The presence of the spike protein led to an increase in Th2 and Th17 cells in peripheral blood and infiltrated damaged tissues, intensifying immune system activation and autoimmune symptoms.
Furthermore, the study highlighted the protein's contribution to the proliferation of effector T cells, particularly Th2 and Th17 cells, which play pivotal roles in autoimmune responses and fibrosis. The exacerbated collagen accumulation and extracellular matrix deposition in skin and lung tissues of SSc mice injected with the spike protein underscored its potential to accelerate fibrosis in the context of SSc.
Delving Deeper: The Interplay Between Immune Cells and Fibroblasts
The intricate pathogenesis of SSc involves a delicate interplay between immune cells and stromal fibroblasts, driving autoimmune dysregulation, fibrosis, and vasculopathy. T cells, particularly when excessively activated, emerge as key players in the aberrant immune response characteristic of SSc. The study's revelations indicate that the SARS-CoV-2 spike protein amplifies the infiltration of Th2 and Th17 cells in the skin and lung tissues of BLM-induced SSc mice.
Classical T helper 2 (Th2) cells, known for secreting cytokines such as IL-4 and IL-13, have long been implicated in promoting fibrosis. Th2 cell profiles, elevated IL-4, and IL-13 levels have been observed in the context of SSc, correlating with disease severity. Additionally, Th17 cells, producers of IL-17, have recently been implicated in SSc pathogenesis, with increased frequency observed in patients correlating with disease activity.
The Cytokine Storm's Role: Inflammatory Response Amplified
SARS-CoV-2 infection triggers a hyperinflammatory response characterized by the rapid and abundant secretion of inflammatory cytokines, a phenomenon commonly referred to as a cytokine storm. This cytokine storm, affecting the functions of immune cells such as macrophages and lymphocytes, coupled with intracellular adhesion molecule dysfunction, increases vascular permeability, facilitating the migration of immune cells into the extracellular matrix.
In this inflammatory environment, macrophages and CD4 T cells stimulate fibroblasts, leading to their proliferation and the synthesis of collagen and matrix metalloproteinases, ultimately resulting in fibrosis and potentially internal organ dysfunction. The study's findings align with this paradigm, suggesting that the SARS-CoV-2 spike protein may contribute to the cytokine storm, further exacerbating the inflammatory response in SSc.
Conclusion: Unraveling the Complexity for Enhanced Patient Care
In conclusion, this in-depth exploration into the impact of the SARS-CoV-2 spike protein on the development and progression of systemic sclerosis provides a crucial piece of the puzzle in understanding the complexities of COVID-19 and autoimmune diseases. The research findings strongly suggest that the SARS-CoV-2 spike protein may indeed expedite the progression of SSc by intensifying fibrosis through the upregulation of inflammation, autoantibody production, and thrombosis.
As the scientific community continues to unravel the intricate connections between COVID-19 and autoimmune diseases, the implications for patient care become increasingly apparent. The need for further investigations is underscored, with questions lingering about the direct influence of the SARS-CoV-2 spike protein on T cell differentiation and the nuanced interactions between immune cells and fibroblasts.
As we navigate the ongoing challenges of the COVID-19 era, the quest for therapeutic interventions to mitigate the impact on individuals with systemic sclerosis gains paramount importance. This study not only deepens our understanding of the intersection between COVID-19 and autoimmune diseases but also beckons a new era of tailored interventions aimed at preserving the well-being of those navigating the complex interplay of these health challenges.
The study findings were published in the peer reviewed Journal of Inflammation.
https://journal-inflammation.biomedcentral.com/articles/10.1186/s12950-023-00362-x
For the latest
COVID-19 News, keep on logging to Thailand Medical News