COVID-19 News: Study Finds Alteration Of Corneal Nerve Parameters And Increase In Dendritic Cells Activation 2 Years After COVID-19 Infection!
Nikhil Prasad Fact checked by:Thailand Medical News Team Oct 13, 2023 1 year, 6 months, 5 days, 15 hours, 47 minutes ago
COVID-19 News: The COVID-19 pandemic, caused by the SARS-CoV-2 virus, has left an indelible mark on global health. While primarily recognized for its respiratory symptoms, COVID-19 has demonstrated its ability to affect virtually all organs in the human body. Among its various manifestations, neurological symptoms such as headaches, fatigue, loss of taste and smell, brain fog, and neuropathic pain have been increasingly documented. Some individuals who recover from the acute phase of the infection continue to experience persistent symptoms, which has been termed Long COVID, as covered in numerous studies, case reports and
COVID-19 News coverages. This complex and heterogeneous condition poses significant challenges to both patients and healthcare providers.
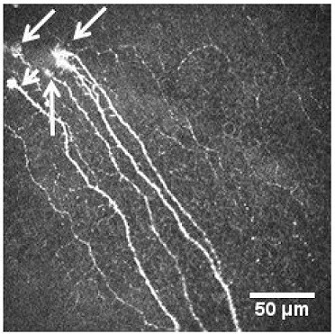
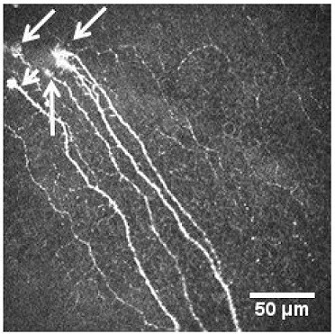 Corneal sub-basal nerve plexus with visible microneuromas marked
Corneal sub-basal nerve plexus with visible microneuromas marked
with arrows. The study team found found the presence of microneuromas
in eyes of about 15% of Long COVID patients!
To delve deeper into the enigmatic realm of Long COVID, a team of researchers from the School of Optometry at the Complutense University of Madrid, Spain, in collaboration with the University of Costa Rica and the Department of Ophthalmology at the Hospital Clínico San Carlos in Spain, conducted a groundbreaking study. This research sought to investigate the corneal nerve parameters and dendritic cell activation in Long COVID patients, focusing on changes occurring over two years after their initial SARS-CoV-2 infection. Their findings may shed light on the potential neuroinflammatory mechanisms underlying Long COVID and the utility of corneal confocal microscopy as a noninvasive diagnostic tool.
Long COVID: A Persistent Enigma
Long COVID, known by various names such as post-COVID conditions (PCC), post-acute sequelae of SARS-CoV-2 infection (PASC), long-haul COVID, and chronic COVID, is characterized by a diverse range of symptoms. The World Health Organization (WHO) defines Long COVID as a condition affecting individuals with a history of probable or confirmed SARS-CoV-2 infection. These individuals typically experience symptoms for at least two months, with onset occurring within three months of the initial infection, and no alternative diagnosis to explain the symptoms.
Fatigue, respiratory distress, and cognitive dysfunction are common among Long COVID patients. Cognitive impairment, including linguistic-cognitive and visual attention deficits, has been increasingly documented, significantly affecting the quality of life and daily activities of Long COVID patients.
Neurological Involvement in Long COVID
The exact mechanisms by which SARS-CoV-2 affects the nervous system are not yet fully understood. However, both innate and adaptive immune responses appear to play a role in the neurological manifestations of the disease. Recent studies have linked Long COVID with small fiber neuropathy (SFN) and peripheral neuropathy. These conditions involve the selective impairment of small, thinly myelinated A-fibers and unmyelinated C-fibers. Interestingly, corneal nerve fiber loss, indicative of neur
odegeneration, is also associated with various other conditions, including fibromyalgia, diabetic neuropathy, and even Alzheimer's disease.
The Cornea as a Window to Neuropathy
The cornea, a highly innervated tissue, receives sensory nerves from the ophthalmic branch of the trigeminal nerve. In addition to sensory fibers, the cornea is supplied with autonomic sympathetic nerve fibers. This intricate innervation network positions the cornea as a unique tissue for noninvasive nerve imaging.
In vivo confocal microscopy (IVCM) is a valuable tool for assessing the peripheral nervous system's integrity. It is particularly useful in the context of neurodegenerative diseases. The cornea, especially its basal epithelium, is home to dendritic cells (DCs), which serve as immune sentinels bridging the innate and adaptive immune responses. DCs also play a role in maintaining corneal nerve homeostasis.
Corneal Microneuromas: Clues to Nerve Regeneration
The study by the Spanish research team revealed the presence of microneuromas in the sub-basal nerve plexus and stromal nerves of Long COVID patients.
Microneuromas, though not fully understood, are believed to form post-nerve injury. They result from the growth of nerve sprouts from the proximal nerve stump, which then advance distally, occasionally growing extraneurally. The formation of microneuromas is associated with neuroinflammatory processes, a mechanism possibly also at play in Long COVID patients.
Corneal Innervation in COVID-19: What We Know
Despite the extensive research into COVID-19, only a few reports have evaluated corneal innervation in patients with the disease. Some studies have indicated reduced corneal nerve fibers and increased dendritic cell presence in both active COVID-19 patients and Long COVID patients three to four months after infection. However, no prior study has investigated individuals with persistent symptoms nearly two years after the initial infection.
The Study's Purpose: Investigating Long COVID
The primary objective of the study conducted by the Spanish research team was to explore the corneal confocal microscopy findings in Long COVID patients who continued to experience symptoms beyond 20 months following their initial SARS-CoV-2 infection. This research aimed to provide insight into the long-term consequences of Long COVID on the corneal nerve parameters and DC activation.
Results of the Study
The research findings unveiled intriguing alterations in the corneal innervation of Long COVID patients, providing significant contributions to our understanding of the condition. Key results from the study include:
-Corneal Nerve Alterations: Long COVID patients exhibited reduced corneal nerve density, shorter corneal nerves, and lower branch densities compared to the control group. These changes suggest a persistent impact of SARS-CoV-2 on the corneal nervous system even two years after infection.
-Dendritic Cell Activation: Long COVID patients displayed an increased density of dendritic cells, along with a greater cell area, in comparison to the control group. The enhanced presence and activation of dendritic cells may signify an ongoing immune response or inflammation within the cornea.
-Microneuromas: Intriguingly, microneuromas were detected in 15% of Long COVID patients, a phenomenon absent in the control group. The presence of microneuromas may be indicative of nerve damage and subsequent regeneration, suggesting a dynamic process within the corneal nerves of Long COVID patients.
Discussion and Implications
The findings of this study suggest that Long COVID has a lasting impact on corneal nerve parameters and dendritic cell activation. The observed alterations in the cornea provide insights into the neuroinflammatory mechanisms potentially underlying Long COVID.
Corneal nerve damage and changes in dendritic cell presence may be linked to a persistent immune response or inflammation, contributing to the neurodegenerative aspects of Long COVID. The presence of microneuromas, while not fully understood, raises questions about the regenerative processes at play within the corneal nerves of Long COVID.
As the research team emphasizes, these results provide a foundation for further investigation. Longitudinal studies and investigations into the impact of treatments on Long COVID patients may reveal additional insights into the condition's pathophysiology.
Conclusion
The study conducted by the School of Optometry at the Complutense University of Madrid, Spain, in collaboration with the University of Costa Rica and the Department of Ophthalmology at the Hospital Clínico San Carlos, Spain, marks a significant step forward in understanding the long-term consequences of Long COVID on the corneal nervous system. The findings of reduced corneal nerve parameters, increased dendritic cell activation, and the presence of microneuromas in Long COVID patients offer vital clues to the neuroinflammatory aspects of this condition.
These results underscore the complexity of Long COVID and its far-reaching effects on the human body, reinforcing the need for continued research and long-term follow-up to provide comprehensive care and management for those affected by this persistent condition. As the world grapples with the aftermath of the COVID-19 pandemic, studies like this contribute to our understanding of the disease's long-term impact and the potential for innovative diagnostic and therapeutic approaches.
The study findings were published in the peer reviewed journal: Diagnostics.
https://www.mdpi.com/2075-4418/13/20/3188
For the latest
COVID-19 News, keep on logging to Thailand Medical News.