COVID-19 News: Study Finds That One Out Of Three COVID-19 Patients Developed Pain 1 Year Later With Fatigue Responsible For Chronicity!
Nikhil Prasad Fact checked by:Thailand Medical News Team Jan 01, 2024 1 year, 3 months, 2 weeks, 1 day, 10 hours, 59 minutes ago
COVID-19 News: The persistent and diverse symptoms of post-COVID-19 syndrome, also known as "long COVID," continue to challenge our understanding of the aftermath of SARS-CoV-2 infection. Among these lingering symptoms, late-onset pain stands out as a significant concern, affecting nearly one-third of patients even a year after their acute infection. Recognizing the need for a deeper understanding of the mechanisms contributing to post-COVID-19 pain, an observational study covered in this
COVID-19 News report, conducted by the University of Ferrara in Italy and Ferrara University Hospital sought to unravel the intricate relationship between fatigue and the development of persistent pain.
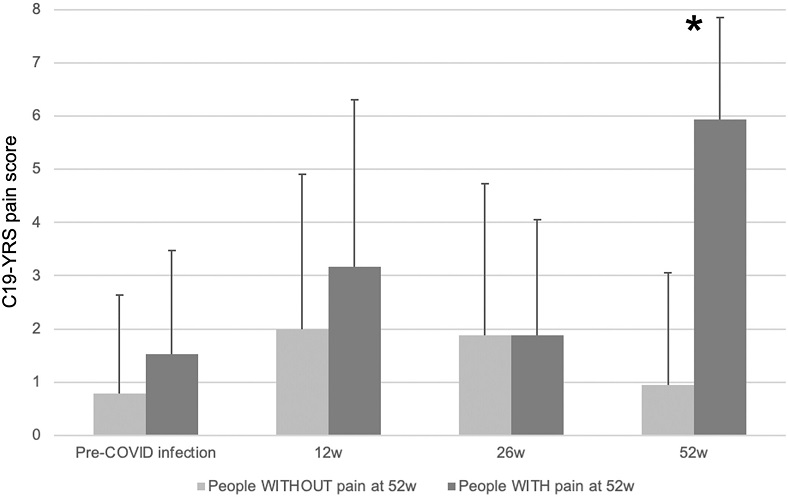
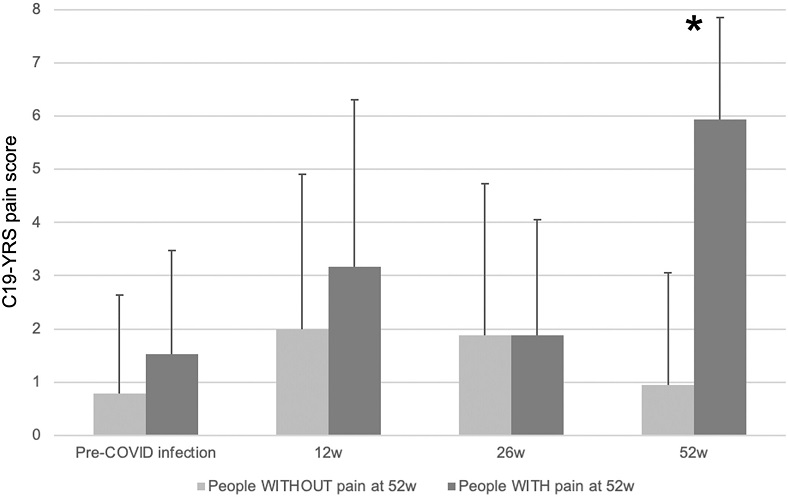 C19-YRS pain score before COVID-19 infection and at the three-time follow-up (12, 26, and 52 weeks) in the two samples. * p < 0.01.
Background - Postacute Sequelae of COVID-19
C19-YRS pain score before COVID-19 infection and at the three-time follow-up (12, 26, and 52 weeks) in the two samples. * p < 0.01.
Background - Postacute Sequelae of COVID-19
COVID-19, caused by the SARS-CoV-2 virus, has not only posed a global health crisis during the acute phase but has also presented challenges in managing postacute sequelae, commonly referred to as "post-COVID-19 syndrome." Beyond the initial respiratory symptoms, survivors have reported a spectrum of persistent issues, including fatigue, dyspnea, cardiovascular complications, and neuropsychiatric disorders. The focus of this study was on the often-overlooked but pervasive problem of post-COVID-19 pain.
Pain as a Lingering Symptom
Pain, as a lingering symptom following SARS-CoV-2 infection, has been a subject of various studies attempting to quantify its prevalence and understand the underlying mechanisms. The prevalence of post-COVID-19 pain in the first year after infection varies widely in the literature, with estimates ranging from 10% to over 60% of individuals experiencing pain during this period. The causes of persistent pain after COVID-19 remain elusive, and proposed pathogenetic mechanisms include nociceptor sensitization due to systemic hyperinflammation and the impact of cytokine storms, potentially leading to neuropathies.
The Need for Precise Evaluation: COVID-19 Yorkshire Rehabilitation Scale (C19-YRS)
To shed light on the nuanced landscape of post-COVID-19 pain, the researchers utilized the COVID-19 Yorkshire Rehabilitation Scale (C19-YRS) as a comprehensive tool for the multidisciplinary assessment of post-COVID-19 syndrome. The C19-YRS, previously used in Italian COVID-19 inpatients, focuses on symptoms and functional difficulties reported by survivors. Its utility extends beyond identifying pain, allowing for a broader understanding of post-COVID-19 sequelae.
Predisposing Factors and Pain Phenotypes
Several predisposing factors for post-COVID-19 pain have been proposed, but consensus remains elusive regarding the mechanisms underlying pain development in the chronic phase. Attempting to categorize pain phenotypes, the study identified three major types: nociceptive, neuropathic, and nociplastic pain. Central sensitization
, proposed as a pathologic mechanism of nociplastic pain, has been hypothesized in post-COVID-19 patients.
Study Methodology and Results
The study enrolled 67 post-COVID-19 patients, assessing their pain intensity using the C19-YRS at 12, 26, and 52 weeks post-infection. Of these patients, 20 exhibited increased pain intensity at the 52-week mark compared to their pre-COVID-19 condition. Strikingly, fatigue emerged as a significant predictor of pain onset (β = 0.54, p = 0.002). Despite similarities in demographic and clinical characteristics at baseline, differences in fatigue, anxiety, mobility, and ability to perform daily activities became apparent at 26 weeks.
The pain assessment revealed 16 different painful body regions, with the shoulder, knee, and lumbar spine being the most frequently affected. Notably, most patients did not exhibit neuropathic or nociplastic mechanisms.
Furthermore, a comparison of pressure pain threshold (PPT) and temporal summation (TS) between patients and healthy controls showed no significant differences.
Discussion: Fatigue as a Key Player
The findings of the study brought attention to the multifaceted relationship between fatigue and post-COVID-19 pain. While previous research has often explored fatigue as a consequence of chronic pain, this study proposed a bidirectional connection, suggesting that fatigue may not only be a result but also a predictor of pain development. This novel perspective challenges the traditional unidirectional understanding of the fatigue-pain relationship.
The fluctuation in pain intensity over the first year post-infection added a layer of complexity to the study's observations. Unlike typical sensitization mechanisms observed in chronic pain syndromes, the pain intensity increased after 12 weeks, decreased at 26 weeks, and then rose again at 52 weeks. This unique temporal pattern raises questions about the development of new mechanisms contributing to pain long after the resolution of the acute infection.
Pain Phenotypes and Mechanisms: A Complex Picture
Efforts to classify post-COVID-19 pain into distinct phenotypes (nociceptive, neuropathic, and nociplastic) revealed challenges in doing so. Pain drawings demonstrated a discrete distribution of symptoms, challenging the notion of widespread pain. Attempts to differentiate between central sensitization and neuropathic pain using specific scoring tools did not provide a clear distinction. The study emphasized the complex and overlapping nature of pain mechanisms in post-COVID-19 patients, suggesting that a single causal mechanism may not fully explain the observed pain experiences.
Implications for Treatment and Prevention
The identification of fatigue as a key predisposing factor for late-onset pain opens new avenues for the development of treatment approaches. While current rehabilitation programs primarily address respiratory symptoms, incorporating aerobic and conditioning strategies may prove beneficial in preventing the development of pain. The comprehensive biopsychosocial model proposed by the study emphasizes the need to address various factors contributing to pain development, creating a holistic approach to therapeutic management.
Limitations and Future Directions
The study acknowledges several limitations, including a relatively small sample size and the absence of specific screening tools for autonomic nervous system dysfunction. Despite these limitations, the research provides valuable insights into the complex interplay between fatigue and post-COVID-19 pain. Future studies with larger cohorts are essential to validate these findings and further explore the intricate relationships among different pain mechanisms in post-COVID-19 patients.
Conclusion
In conclusion, this observational study adds depth to our understanding of post-COVID-19 pain by unraveling the intricate relationship between fatigue and the development of persistent pain. While fatigue emerges as a significant predictor of late-onset pain, the study underscores the need for a comprehensive approach that considers overlapping pain mechanisms and addresses predisposing factors. These findings provide valuable insights for the development of new strategies in the prevention and treatment of post-COVID-19 pain, particularly where fatigue and impaired daily activities play pivotal roles. As our understanding evolves, these insights pave the way for more targeted and effective interventions to improve the quality of life for post-COVID-19 survivors grappling with persistent pain.
The study findings were published in the peer reviewed European Journal of Pain.
https://onlinelibrary.wiley.com/doi/10.1002/ejp.2228
For the latest
COVID-19 News, keep on logging to Thailand Medical News.