COVID-19 News: Study Uncovers The Role Of Anti-Phospholipid Antibodies In Thrombosis And Hyperinflammation During COVID-19 Acute Phase
Thailand Medical News Team Aug 20, 2023 2 years, 5 months, 2 weeks, 1 day, 7 hours, 54 minutes ago
COVID-19 News: In the wake of the emergence of the severe acute respiratory distress syndrome coronavirus-2 (SARS-CoV-2) virus, the world witnessed the rapid spread of coronavirus disease 2019 (COVID-19), marked by diverse clinical presentations ranging from mild respiratory symptoms to severe respiratory distress and systemic complications. The virus's propensity to induce coagulopathy has become increasingly evident through various hemostatic laboratory indicators as published in various studies and
COVID-19 News reports. The coexistence of microthrombosis, thrombosis, and thromboembolic events in fatal COVID-19 cases has underscored the significance of clotting abnormalities in the disease's pathophysiology.
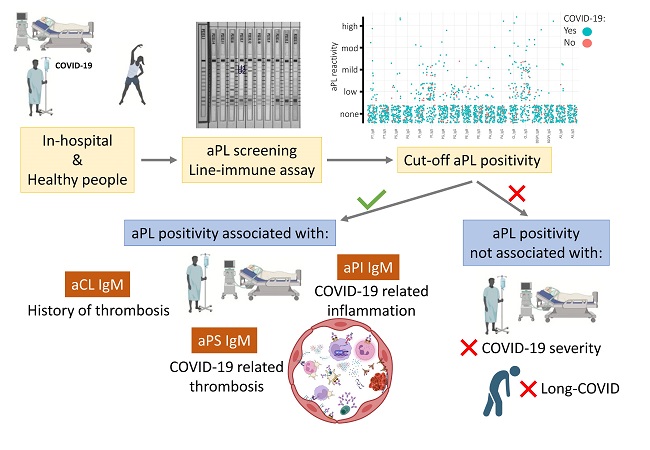
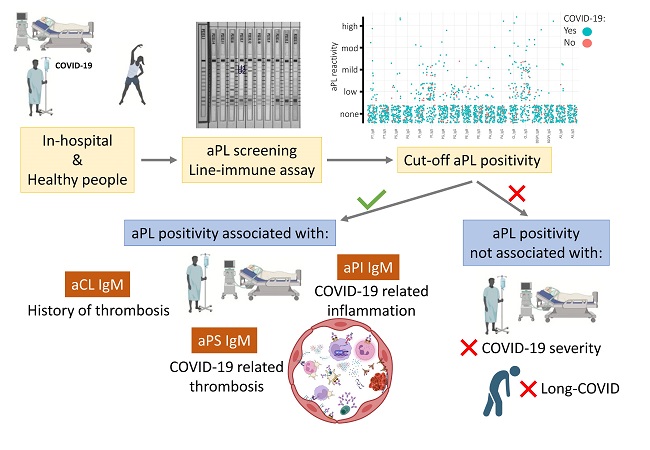 Graphical Abstract
Graphical Abstract
Of particular interest is the intricate interplay between inflammation and clotting pathways in the context of COVID-19. Inflammatory responses are provoked when tissues undergo damage or infection, triggering the release of signaling molecules like cytokines and chemokines. These molecules not only summon immune cells to the site of injury but also activate clotting and complement pathways. Immune cells, especially neutrophils and monocytes, release procoagulant substances and serine proteases, fostering clot formation.
Conversely, inflammatory molecules can activate platelets and promote their aggregation. Clotting factors like thrombin can directly activate immune cells and stimulate the release of inflammatory mediators.
Within this complex web of interactions, the role of antiphospholipid antibodies (APLA) comes into play. APLA encompass a diverse group of antibodies targeting various phospholipids. These antibodies have the potential to activate clotting and complement pathways, thereby contributing to thrombotic events. While some APLA, like anti-cardiolipin (aCL) and anti-β2-Glycoprotein I (aβ2GPI), play a central role in antiphospholipid syndrome (APS), a condition characterized by thrombotic events, other non-criteria APLA are less understood. The intriguing connection between COVID-19 and APLA has prompted researchers to explore their prevalence and impact in COVID-19 patients.
In a study conducted during the initial pandemic outbreak in Catalonia-Spain, the study team investigated the relationship between APLA positivity and COVID-19-related thrombosis, inflammation, disease severity, and long COVID-19 outcomes.
The study enrolled 92 hospitalized COVID-19 patients and tested them for 18 different APLAs using a single line-immunoassay (LIA) test. The prevalence of APLA positivity was found to be approximately 32.61%, and 10
.87% of patients exhibited positivity for more than one APLA.
Among the various APLAs tested, anti-phosphatidylserine (aPS) IgM positivity was associated with thrombosis occurrence in COVID-19 patients. On the other hand, anti-phosphatidylinositol (aPI) IgM positivity was linked to higher levels of the inflammatory marker interleukin-6 (IL-6) and ferritin.
Interestingly, while thrombosis and inflammation were associated with specific APLAs, none of the APLA positivities correlated with disease severity or the likelihood of experiencing long COVID-19 symptoms.
It is worth noting that antiphospholipid antibodies induced by viral infections have been recognized in the past, suggesting that SARS-CoV-2, as a virus, might also induce the production of these antibodies. However, the exact role and persistence of such antibodies in COVID-19 are yet to be fully elucidated. The study's findings contribute to the growing body of evidence suggesting that certain APLA positivities, particularly aPS IgM and aPI IgM, could serve as markers for thrombotic events and hyperinflammatory states in COVID-19 patients.
Despite the intriguing insights provided by this study, some limitations must be acknowledged. The study did not test for lupus anticoagulant (LA), a particular type of APLA. Additionally, follow-up data over an extended period were not available to determine the persistence of APLA positivity and its potential impact on long COVID-19 outcomes.
In conclusion, the study sheds light on the role of specific non-criteria APLAs, aPS IgM, and aPI IgM, in COVID-19-related thrombosis and hyperinflammation. While APLA positivities were not predictive of disease severity or long COVID-19, their association with specific clinical complications offers valuable insights for patient management. These findings underscore the importance of considering APLA testing, beyond standard criteria APLAs, as a means to assess the risk of thrombosis and inflammation in hospitalized COVID-19 patients. As research into the intricate mechanisms underlying COVID-19 continues, these findings contribute to our understanding of the disease's complex pathophysiology and offer potential avenues for improved clinical care and management strategies. Further studies are warranted to confirm these associations and uncover additional nuances in the role of APLAs in COVID-19.
The study findings were published in the peer reviewed journal: Biomedicine.
https://www.mdpi.com/2227-9059/11/8/2301
For the latest
COVID-19 News, keep on logging to Thailand Medical News.