COVID-19 News: Study Uncovers The Role Of Macrophage Migration Inhibitory Factor Receptor CD74 In T Cell Immune Responses To SARS-CoV-2
Nikhil Prasad Fact checked by:Thailand Medical News Team Oct 29, 2023 2 years, 3 months, 1 week, 9 hours, 57 minutes ago
COVID-19 News: The COVID-19 pandemic, driven by the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), has left an indelible mark on the world with millions of cases and deaths reported worldwide. The severity of pulmonary pathologies and poor prognosis in COVID-19 patients has been linked to the activation of non-virus-specific bystander T cells. Additionally, high concentrations of the macrophage migration inhibitory factor (MIF) have been identified in the serum of COVID-19 patients. This raises questions about the potential relationship between these two pathogenic factors and their impact on the immune response to the virus.
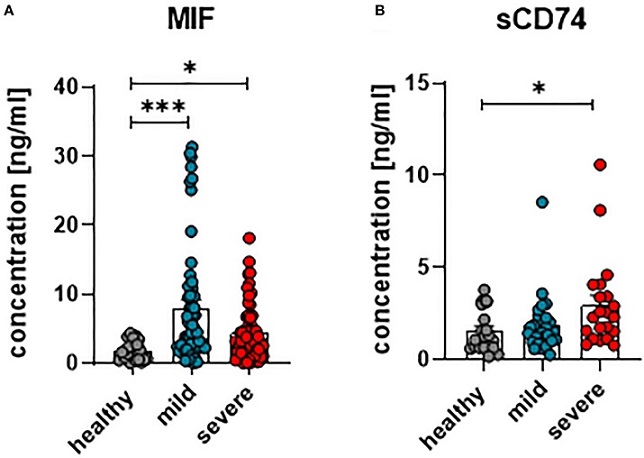
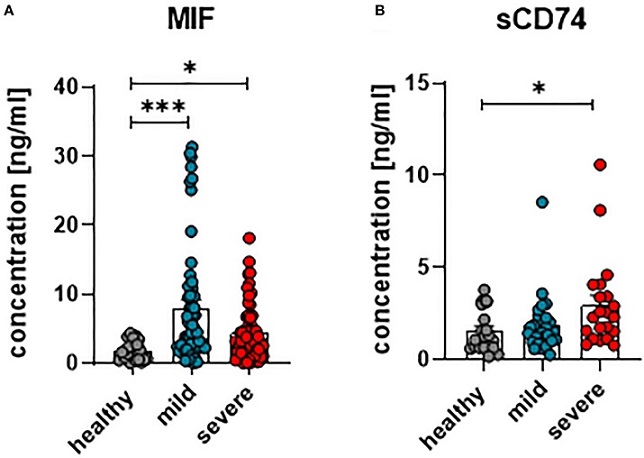 Concentrations of plasma MIF and sCD74 in COVID-19. The concentration of MIF (A) and sCD74 (B) in the plasma of patients with mild or severe COVID-19 and healthy donors were measured by ELISA. Each dot represents an individual patient. Statistically significant differences are indicated by asterisks (* < 0.05; *** < 0.001).
Concentrations of plasma MIF and sCD74 in COVID-19. The concentration of MIF (A) and sCD74 (B) in the plasma of patients with mild or severe COVID-19 and healthy donors were measured by ELISA. Each dot represents an individual patient. Statistically significant differences are indicated by asterisks (* < 0.05; *** < 0.001).
In this
COVID-19 News report, we delve into a study conducted by a consortium of esteemed institutions including the University of Duisburg-Essen in Germany, the University Hospital of the Ruhr-University Bochum in Germany, Huazhong University of Science and Technology (HUST) in China, University Hospital Essen in Germany, Friedrich-Alexander-Universität Erlangen-Nürnberg in Germany, Poltava State Medical University in Ukraine, and Charité - Universitätsmedizin Berlin in Germany. The study's focus is on the expression of receptors for MIF on T cells in COVID-19 patients and the implications for the expansion and differentiation of effector T cells.
Understanding the Complex Dynamics of COVID-19
The COVID-19 pandemic is characterized by the infection of lung epithelial cells, leading to pneumonia and a cascade of immune responses that result in acute progressive pneumonia. This condition contributes to reduced oxygen saturation in the blood and exacerbates disease progression in COVID-19 patients. The death of infected lung epithelial cells triggers the production of various inflammatory proteins such as MIP1α, MIP1β, MCP1, IL-6, and IP-10 in neighboring cells, driving inflammation and the migration of immune cells into the infected areas.
Moreover, patients with severe COVID-19 exhibit elevated levels of Macrophage Migration Inhibitory Factor (MIF) in their serum, which is associated with the progression of the disease. Elevated MIF levels have also been observed in other respiratory conditions like asthma and lung fibrosis.
MIF's Role in COVID-19
Macrophage Migration Inhibitory Factor (MIF) is a multifunctional molecule with various roles, including enzymatic activity, countering the effects of immunosuppressive glucocorticoids, and recruiting hematopoietic cells to sites of tissue damage.
MIF has been implicated in sustaining pulmonary inflammation in the acute respiratory distress syndrome (ARDS) and is associated with numerous inflammatory lung diseases. Notably, a polymorphism an
alysis of MIF promoter alleles has linked COVID-19 progression to the increased expression of a specific MIF allele in patients. The interaction of MIF with its receptor, CD74, is crucial for signal transduction. CD74, also known as the MHC class II chaperone invariant chain, lacks an intrinsic intracellular signaling domain. It relies on the formation of complexes with co-receptors such as CD44, CXCR2, and CXCR4 to induce intracellular signaling. The presence of these receptors on various immune cells, including T cells, raises questions about their role in SARS-CoV-2 infections.
The Role of T Cells in COVID-19
Both CD4+ and CD8+ T cells play pivotal roles in recognizing different epitopes of SARS-CoV-2, contributing to viral control. However, an uncontrolled immune response can lead to inflammation in infected organs, potentially causing severe pathologies. Bystander T cells, which do not respond to viral antigens but to antigen-independent signals like inflammatory cytokines, have been associated with COVID-19 severity. In this study, the researchers sought to characterize CD4+ and CD8+ T cells in terms of their expression of receptors that recognize MIF. This approach aimed to elucidate the role of MIF in COVID-19 immunopathology and understand the interplay between MIF and bystander T cells.
Expression of MIF Receptors on T Cells
The study revealed a significant increase in the proportion of CD4+ and CD8+ T cells expressing CD74 on the cell surface in COVID-19 patients compared to healthy controls. To induce intracellular signaling upon MIF binding, CD74 forms complexes with CD44, CXCR2, or CXCR4. Most CD74+ T cells expressed CD44, with the expression of CXCR2 and CXCR4 being low in healthy controls but increasing upon SARS-CoV-2 infection. This indicates that T cells in COVID-19 patients express receptors that render them responsive to MIF.
Differential T Cell Phenotypes
A detailed analysis of CD74+ T cell populations revealed that most of them had a central memory phenotype early in the infection, while cells with effector and effector memory phenotypes emerged later during the infection. Furthermore, CD74+ T cells produced more cytotoxic molecules and proliferation markers. This suggests that MIF may play a crucial role in the activation and expansion of effector T cells in COVID-19.
Implications for COVID-19 Pathogenesis
The study's findings shed light on the potential regulatory role of MIF in bystander T cell activation during COVID-19. The presence of MIF receptors on T cells, combined with elevated MIF levels in the plasma of COVID-19 patients, suggests a complex interplay that influences disease progression and severity. Activated bystander T cells, especially CD8+ T cells, can produce pro-inflammatory cytokines and cytotoxic molecules. The expansion and accumulation of these cells in infected organs, particularly the lungs, may contribute to immunopathology in COVID-19 patients. Given that MIF signaling can affect the large population of bystander T cells, targeting the MIF system with therapeutic interventions may hold promise in reducing the severity of the disease and protecting infected organs.
Conclusion
The COVID-19 pandemic has brought to light the intricate dynamics between the SARS-CoV-2 virus and the host immune system. Bystander T cells, which do not respond to viral antigens but become activated by antigen-independent signals, play a significant role in the immunopathology of the disease. This study's findings indicate that MIF, a pro-inflammatory cytokine, and its receptor CD74 are intricately involved in the activation and expansion of effector T cells during COVID-19. As MIF is elevated in the serum of COVID-19 patients and CD74 is expressed on T cells, this opens up new avenues for research and potential therapeutic interventions. Understanding the complex interplay between MIF and T cells is crucial for developing strategies to mitigate the severity of COVID-19 and protect infected organs. Future research may focus on the development of drugs, peptides, and antibodies targeting MIF and CD74, potentially offering new immunotherapies for COVID-19 and other inflammatory immunopathologies. The role of MIF in COVID-19 pathogenesis continues to be a subject of intense investigation, holding promise for improved treatments and outcomes in the ongoing battle against this global health crisis.
The study findings were published in the peer reviewed journal: Frontiers in Immunology.
https://www.frontiersin.org/articles/10.3389/fimmu.2023.1236374/full
For the latest
COVID-19 News, keep on logging to Thailand Medical News.