COVID-19 News: Turkish Study Shows That COVID-19 Can Cause Miller Fisher Syndrome As A Result Of Molecular Mimicry!
Nikhil Prasad Fact checked by:Thailand Medical News Team Sep 12, 2023 1 year, 7 months, 1 week, 1 day, 1 hour, 56 minutes ago
COVID-19 News: In a groundbreaking development, a recent Turkish study conducted at Izmir University has unearthed a startling revelation: COVID-19 may trigger Miller Fisher Syndrome (MFS) through a phenomenon known as molecular mimicry. Miller Fisher Syndrome or MFS, a rare neurological disorder falling under the Guillain-Barré syndrome (GBS) spectrum, manifests as muscle weakness and results from an immune system reaction targeting specific nerve proteins crucial for sensory and motor functions. This autoimmune condition stems from antibodies launched against bacterial or viral infections that inadvertently assault nerve structures, such as myelin sheaths or axons.
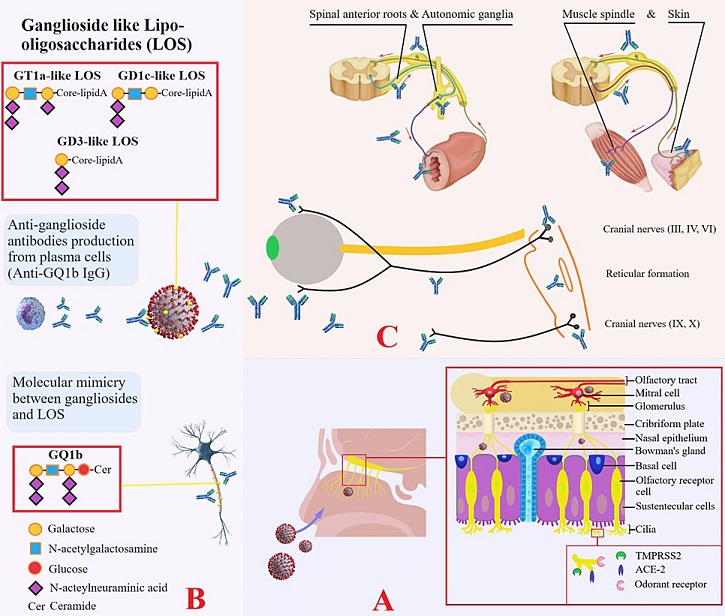
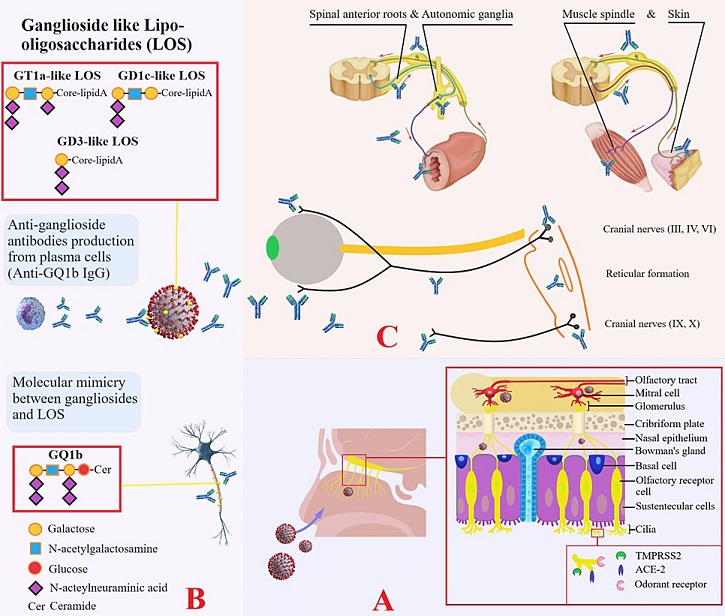 Mechanism of molecular mimicry in Miller Fisher syndrome associated with COVID-19
Mechanism of molecular mimicry in Miller Fisher syndrome associated with COVID-19
Panel A: Demonstrates transcribrial neurotropism of SARS-CoV-2 via ciliary chemoreceptors (TMPRSS2 and ACE-2 receptors) in the olfactory epithelium and neuroinvasion via olfactory tractus. Panel B: Demonstrates the mechanism of molecular mimicry between central and peripheral paranodal neuronal ganglioside epitopes and ganglioside-like lipo-oligosaccharides of the virus. Panel C: Demonstrates the antigenic targets of antibodies produced by plasma cells: muscle spindles; autonomic preganglionic, ganglionic, and postganglionic fibers; spinal anterior roots; third, fourth, and sixth cranial nerves; reticular formation; and ninth and 10th cranial nerves. The clinical features that occur as a result of the effects of these regions constitute Miller Fisher syndrome.
An earlier
COVID-19 News report in Thailand Medical News in August 2020 also warned that COVID-19 could lead to the manifestation of Miller Fisher Syndrome.
https://www.thailandmedical.news/news/breaking-neuro-covid-researchers-warn-of-new-neurological-conditions-manifesting-in-covid-19-patients-miller-fisher-syndrome-and-polyneuritis-craniali
MFS's origins trace back to its identification in 1932, presenting as a triad of ataxia, ophthalmoplegia, and areflexia. Subsequently, a leading neurologist, Dr Miller Fisher spotlighted this triad as a distinct variant of GBS in 1956, resulting in the syndrome bearing his name. Amid the ongoing SARS-CoV-2 pandemic, reports of both peripheral and central nervous system involvement have surfaced. Until December 2022, 24 cases, including four in children, were documented linking MFS to COVID-19. This new study review delves into the basic clinical and laboratory characteristics of these patients and the proposed molecular mimicry mechanism while acknowledging the need for further research to solidify this connection.
Background
MFS, marked by its classic triad, is a relatively rare neuropathy, with an incidence of 5% among GBS cases. Diagnostic markers include normal white blood cell counts but elevated protein levels in cerebrospinal fluid (CSF), termed albuminocytological dissociation (ACD), and the presence of anti-GQ1b IgG antib
odies against ganglioside GQ1b. Electroneuromyography (ENMG) and magnetic resonance imaging (MRI) can provide further diagnostic insights.
COVID-19, caused by SARS-CoV-2, was declared a pandemic in March 2020, unleashing a multitude of neurological symptoms and complications. While common symptoms include anosmia, ageusia, and headaches, severe outcomes such as stroke, seizures, and encephalopathy have also been reported.
As of January 2023, 25 cases of COVID-19-associated MFS have been documented, with diverse clinical presentations. Notably, some cases with mild COVID-19 symptoms exhibited MFS, highlighting its potential occurrence irrespective of the severity of the viral infection. While this article reviews existing case reports, a deeper understanding hinges on larger epidemiological studies.
Study Findings And Implications
Among the 25 COVID-19-associated MFS cases, the majority (76%) were male, with a median age of 40.32 years. These cases spanned nine countries, primarily Europe and the USA. While the majority of patients received a COVID-19 diagnosis before MFS onset, a few discovered their infection during hospitalization for MFS.
Notable COVID-19 symptoms included fever and respiratory complaints.
Neurological manifestations, including areflexia, ophthalmoparesis, and ataxia, appeared approximately two weeks post-COVID-19 diagnosis or symptom onset. ENMG revealed various abnormalities, while ACD was present in most CSF analyses. Anti-GQ1b antibodies were positive in a subset of cases, but not universally.
MFS is chiefly characterized by its classical triad of symptoms. While some COVID-19-related MFS cases are severe, others present with mild COVID-19 symptoms or are asymptomatic, emphasizing its potential in any SARS-CoV-2-exposed individual.
While this study reviews clinical features based on case reports, larger epidemiological studies are pivotal in establishing a concrete link between COVID-19 and MFS. With COVID-19's ongoing evolution, continued research is essential to explore its neurological impact and the underlying mechanisms.
Molecular mimicry, the proposed pathogenic mechanism, arises from antecedent infections, with Campylobacter jejuni and Hemophilus influenza being common culprits. However, numerous pathogens, including Cytomegalovirus, Mycoplasma pneumoniae, and Varicella zoster, have also been associated. COVID-19's emergence has added to the list of microbes linked to MFS, raising questions about the role of vaccines in its development.
Mechanism of Molecular Mimicry in COVID-19-Associated MFS
Molecular mimicry involves the adaptive immune system and the resemblance between peripheral nerve and microbial/viral antigens. Research has shown that anti-GQ1b antibodies may be present in MFS, leading to conduction block in nerves. Notably, anti-GQ1b antibodies were frequently positive in COVID-19-related MFS cases, whereas they were less common in non-COVID-19 MFS cases. This discrepancy suggests the involvement of alternative mechanisms or receptors in the neuropathogenesis of COVID-19-associated MFS.
While anti-GQ1b antibodies play a crucial role in diagnosing non-COVID-19 MFS, they appear less reliable in COVID-19-related cases. Instead, ACD in CSF and EMG examinations seem to offer more diagnostic value for COVID-19-associated MFS. These findings highlight the complexity of diagnosing and understanding this condition, particularly in the context of COVID-19.
Treatment and Prognosis
Though MFS is usually self-limiting with a favorable prognosis, severe cases can lead to complications like pulmonary arrhythmia and respiratory failure. Ophthalmoplegia and ataxia typically improve within one to three months. Treatment options, including plasma exchange and intravenous immunoglobulin, may be considered in more severe cases. However, MFS often follows a spontaneous remission trajectory.
Conclusion
In conclusion, this new study sheds light on a compelling link between COVID-19 and Miller Fisher Syndrome, driven by molecular mimicry. While the evidence is compelling, larger-scale epidemiological research is needed to solidify this connection and understand the full scope of neurological complications associated with COVID-19. The discovery of ACD in CSF and the presence of EMG abnormalities emerge as valuable diagnostic markers in COVID-19-related MFS. As the world grapples with the ongoing pandemic and the evolving landscape of viral variants, continued research will be crucial in unraveling the mysteries surrounding COVID-19's impact on the nervous system and its potential to trigger rare autoimmune conditions like MFS.
The study findings were published in the peer reviewed journal: Cureus.
https://www.cureus.com/articles/171629-miller-fisher-syndrome-associated-with-covid-19-a-history-of-molecular-mimicry-and-an-up-to-date-review-of-the-literature#!/
For the latest
COVID-19 News, keep on logging to Thailand Medical News.