COVID-19 News: U.S. Study Using Human Intranasal Micro-Optical Coherence Tomography Imaging Validates That COVID-19 Causes Ciliary Dysfunction
Nikhil Prasad Fact checked by:Thailand Medical News Team Nov 05, 2023 1 year, 5 months, 1 week, 6 days, 15 hours, 14 minutes ago
COVID-19 News: The COVID-19 pandemic has undoubtedly reshaped the way we view and understand infectious diseases. As the world continues to grapple with the challenges posed by the novel coronavirus, dedicated researchers and medical professionals are working tirelessly to shed light on various aspects of the virus's behavior.
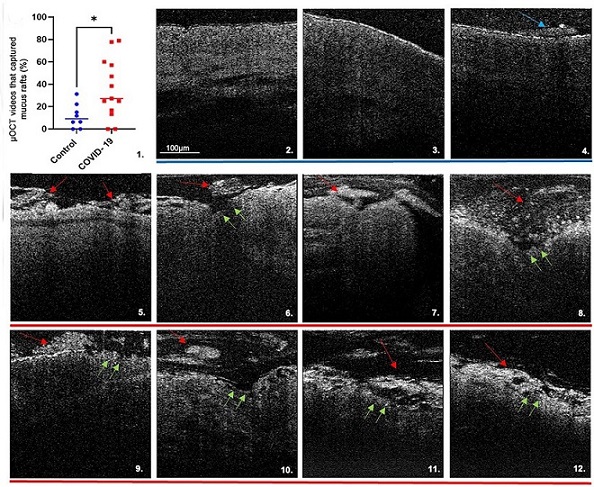
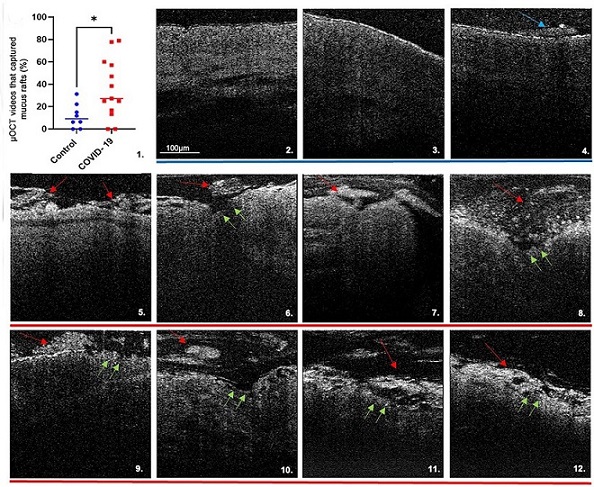 Micro-optical coherence tomography (μOCT) imaging and results. Demonstrates multiple μOCT imaging abnormalities in subjects with COVID-19. (C.1) Scatter plot with increased prevalence of mucus rafts in patients with COVID-19 are shown (11.6% ± 10.9% healthy control subjects [blue dots] vs. 35.9% ± 26.7% patients with COVID-19 [red dots]; P = 0.0282.) Each data point represents the mean measurement of percentage of μOCT videos with mucus rafts identified per subject. Bars indicate means; comparison of data by Mann-Whitney test: *P < 0.05. Healthy control subjects (C.2–C.4) with uniform PCL layer, preserved epithelium, and minimal mucus accumulation (blue arrows), versus subjects with COVID-19 (C.5–C.12) with larger and more readily apparent mucus rafts (red arrows), denuded epithelium, and loss of ciliary coverage (green arrows). CBF = ciliary beat frequency; HEPA = high efficiency particulate air; MCT = mucociliary transport rate; pCC = percent ciliary coverage.
Micro-optical coherence tomography (μOCT) imaging and results. Demonstrates multiple μOCT imaging abnormalities in subjects with COVID-19. (C.1) Scatter plot with increased prevalence of mucus rafts in patients with COVID-19 are shown (11.6% ± 10.9% healthy control subjects [blue dots] vs. 35.9% ± 26.7% patients with COVID-19 [red dots]; P = 0.0282.) Each data point represents the mean measurement of percentage of μOCT videos with mucus rafts identified per subject. Bars indicate means; comparison of data by Mann-Whitney test: *P < 0.05. Healthy control subjects (C.2–C.4) with uniform PCL layer, preserved epithelium, and minimal mucus accumulation (blue arrows), versus subjects with COVID-19 (C.5–C.12) with larger and more readily apparent mucus rafts (red arrows), denuded epithelium, and loss of ciliary coverage (green arrows). CBF = ciliary beat frequency; HEPA = high efficiency particulate air; MCT = mucociliary transport rate; pCC = percent ciliary coverage.
In a groundbreaking study conducted in the United States that is covered in this
COVID-19 News report, scientists explored the impact of COVID-19 on the ciliated nasal epithelium using Intranasal Micro-Optical Coherence Tomography Imaging (μOCT). The study was a collaborative effort involving the University of Alabama at Birmingham, the Gregory Fleming James Cystic Fibrosis Research Center, Massachusetts General Hospital, Harvard Medical School, Healthcare Innovation Partners, and ELEVEN, LLC. The results of this study offer profound insights into the impact of COVID-19 on respiratory health, with implications for our understanding of disease transmission and potential treatments.
The Nasal Epithelium and SARS-CoV-2
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), responsible for COVID-19, primarily gains entry to the human body through the respiratory system. It does so by binding to ACE2 receptors, which are highly expressed in the ciliated cells of the nasal epithelium. The nasal epithelium serves as a vital barrier, responsible for filtering and trapping pathogens, such as viruses and bacteria. It is lined with cilia – tiny, hair-like structures - that play a crucial role in moving mucus and trapped particles out of the airways. Any dysfunction in this system can have significant implications for respiratory health.
Micro-Optical Coherence Tomography (μOCT)
Micro-Optical Coherence Tomography (μOCT) is an innovative, minimally invasive imaging technique that allows for the visualization and quantification
of epithelial anatomy, ciliary motion, and mucus transport within the respiratory tract. In this study, researchers aimed to use μOCT to investigate the functional dynamics of the nasal epithelium in individuals with COVID-19, with a particular focus on ciliary function and mucociliary abnormalities.
Hypothesis and Study Design
The researchers hypothesized that COVID-19 would manifest as reduced ciliated cell function and mucociliary abnormalities, which could be readily visualized using μOCT. To test this hypothesis, the study recruited symptomatic outpatients aged 18 years and older who had tested positive for SARS-CoV-2 within 14 days of the onset of symptoms. The μOCT imaging was conducted within a custom-designed negative-pressure isolation booth to minimize the risk of virus transmission.
Key Findings
The study's findings provided a comprehensive view of the impact of COVID-19 on the nasal epithelium and ciliary function:
Mucus Accumulation and Epithelial Disruption: μOCT imaging identified significant mucus accumulation, denuded epithelium (the loss of the protective cell layer), and increased immune cell infiltration in COVID-19 patients. Mucus, secreted in response to infection, often formed mucus plaques or "mucus rafts" under pathological conditions. The presence of mucus rafts was significantly higher in COVID-19 patients, indicating a strong association between mucus hypersecretion and underlying epithelial injury.
Loss of Ciliary Coverage and Ciliary Dysfunction: COVID-19 patients exhibited a severe reduction in ciliary coverage, a reduced ciliary beat frequency (CBF), and irregular ciliary beat patterns. These results demonstrated the profound impact of the virus on ciliated cell function within the nasal epithelium. The loss of coordinated motion and compromised ciliary function can hinder the effective removal of mucus and pathogens from the respiratory tract.
Discussion
The findings of this study carry significant implications for our understanding of COVID-19 and its impact on respiratory health. Cilia are crucial for maintaining the health of the respiratory system, as they play a central role in clearing mucus and pathogens. The study's results suggest that even individuals with mild COVID-19 symptoms experience severe ciliated cell abnormalities and functional deficiencies within the mucociliary apparatus.
Moreover, these findings add to the growing body of evidence that ciliary injury is a common feature in various COVID-19 models, with in vitro and in vivo studies consistently showing abnormalities in ciliary function and mucociliary clearance. Importantly, these disruptions were observed in COVID-19 patients with mild symptoms, underscoring the need to further explore the role of ciliated cells early in the disease process to mitigate SARS-CoV-2 transmission.
Limitations and Future Research
It's essential to acknowledge the limitations of this study, primarily its small sample size and the lack of longitudinal data on disease progression and complications. As the study focused on individuals with mild symptoms and self-limited courses of the disease, more extensive research is needed to understand the broader implications of ciliary dysfunction in COVID-19. Additionally, the inability to perform serial imaging throughout the disease course and obtain invasive biopsies restricts a comprehensive understanding of the disease's progression and histopathological correlations.
Conclusion
The U.S. study using Intranasal Micro-Optical Coherence Tomography Imaging has provided critical insights into the impact of COVID-19 on the nasal epithelium and ciliary function. The findings highlight the importance of maintaining mucociliary health, even in individuals with mild COVID-19 symptoms, and suggest that ciliary imaging could be a valuable tool for evaluating disease progression and therapeutic response.
As the world continues to grapple with the COVID-19 pandemic, research efforts like this one are essential for advancing our understanding of the virus and developing more effective strategies for prevention and treatment. The study's results emphasize the need to explore ciliary cells as a potential target for mitigating disease transmission and underscore the applicability of ciliary imaging in the study of other viral respiratory disorders. Ultimately, this research brings us one step closer to unraveling the mysteries of COVID-19 and developing more effective interventions for this global health crisis.
The study findings were published in the peer reviewed journal: American Journal of Respiratory Cell and Molecular Biology.
https://www.atsjournals.org/doi/full/10.1165/rcmb.2023-0177LE
For the latest
COVID-19 News, keep on logging to Thailand Medical News.