COVID-19 News: While Lymphopenia Is Common In SARS-CoV-2 Infections, Some May Suffer From B Cell Lymphocytosis, That Leads To Lymphocytic Leukemia!
COVID-19 News - B Cell Lymphocytosis - as chronic lymphocytic leukemia Feb 14, 2023 2 years, 2 months, 3 days, 16 hours, 58 minutes ago
COVID-19 News: Researchers from University of Genoa-Italy, S. Paolo Hospital, Savona-Italy, IRCCS Istituto Giannina Gaslini-Italy, Santa Corona Hospital, Pietra Ligure-Italy and IRCCS Ospedale Policlinico San Martino-Italy have in a news study found that a sub-group of patients infected with SARS-CoV-2 can end up with CD5+ B Cell Lymphocytosis that can end up as chronic lymphocytic leukemia, although majority of COVID-19 patients typically display lymphopenia.
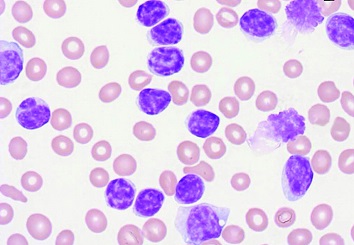
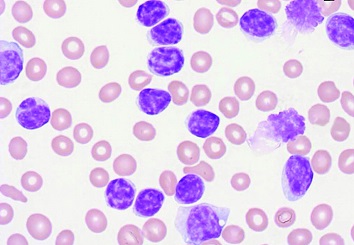 B-Cell-Lymphocytosis
B-Cell-Lymphocytosis
B-cell lymphocytosis (MBL) is an asymptomatic condition in which individuals have increased blood levels of particular subtypes of monoclonal lymphocytes (i.e. an aberrant and potentially malignant group of lymphocytes produced by a single ancestral cell).
Chronic lymphocytic leukemia (CLL) is a type of cancer that starts from white blood cells (called lymphocytes) in the bone marrow.
According to the study team, recently, cases of fortuitous discovery of Chronic Lymphocytic Leukemia (CLL) during hospitalization for Coronavirus disease (COVID-19) have been reported.
Alarmingly, these patients did not show a monoclonal B cell expansion before COVID-19 but were diagnosed with CLL upon a sudden lymphocytosis that occurred during hospitalization.
The (hyper)lymphocytosis during COVID-19 was also described in patients with overt CLL disease. Contextually, lymphocytosis is an unexpected phenomenon since it is an uncommon feature in the COVID-19 patient population, who rather tend to experience lymphopenia. Thus, lymphocytosis that arises during COVID-19 infection is a thought-provoking behavior, strikingly in contrast with that observed in non-CLL individuals.
The study team speculates about the possible mechanisms involved with the observed phenomenon. Many of the plausible explanations might have an adverse impact on these CLL patients and further clinical and laboratory investigations might be warranted.
The study findings were published in the peer reviewed Journal of Clinical Medicine.
https://www.mdpi.com/2077-0383/12/3/998
Already a number of studies that were not covered in any
COVID-19 News coverages have indicated that SARS-CoV-2 infections can cause B Cell Lymphocytosis in some.
https://www.frontiersin.org/articles/10.3389/fonc.2020.582901/full
https://pubmed.ncbi.nlm.nih.gov/35352666/
https://pesquisa.bvsalud.org/global-literature-on-novel-coronavirus-2019-ncov/resource/pt/covidwho-1092793
Typically, most COVID-19 patients display overt lymphopenia, which is associated with CD4+ and CD8+ T cell activation and proliferation, cy
tokine serum levels increase (e.g., IL-1RA IL-6, IL-8, IL-10, and CXCL10), and T-bet+ with decreased CXCR5 B cells. Hence, SARS-CoV-2 infection can trigger a complex crosstalk of the immune system.
However, B Cell Lymphocytosis though rare in COVID-19 individuals, seems to be occurring more with the advent of the newer SARS-CoV-2 variants and sub-lineages!
Chronic lymphocytic leukemia (CLL), the most common B cell leukemia in adult Caucasians, is characterized by the expansion of a monoclonal population of CD5+ B lymphocytes.
To date, it is not fully clear whether SARS-CoV-2 infection in CLL patients leads, on average, to worse or milder COVID-19 symptomatology compared to age-matched healthy individuals or groups with other comorbidities.
Both options are reported and appear linked to (i) the CLL stage, (ii) undergoing CLL treatment, and (iii) the type of treatment.
In the same light, the effects of SARS-CoV-2 infection on CLL pathogenesis and clinical evolution are also unclear. Herein, the study team specifically address the latter issue, based on the available evidence, and try to propose the most likely mechanisms involved.
The study team recently described a clinical case that presented to the emergency with SARS-CoV-2 infection symptoms.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9073957/
The patient was admitted with a normal blood cell count. Two days later, a rapid and unexpected increase in the lymphocyte count led to further investigations that highlighted a population of CD5+ monoclonal B cells with a count above clinical parameters for chronic lymphocytic leukemia (CLL), leading to a new CLL diagnosis.
The study team also found other anecdotal cases of fortuitous discovery of CLL during hospitalization for COVID-19.
https://www.cureus.com/articles/90890-emergence-of-chronic-lymphocytic-leukemia-during-admission-for-covid-19-cause-or-coincidence#!/
https://pubmed.ncbi.nlm.nih.gov/33098641/
https://pubmed.ncbi.nlm.nih.gov/33161639/
All these patients did not show a monoclonal B cell expansion before COVID-19 but were diagnosed with CLL upon a sudden lymphocytosis that occurred during hospitalization. The lymphocytosis associated with the emergence of a CD5+ monoclonal B cell expansion is referable to CLL.
Interestingly, in all these cases, the leukemic clone persisted after recovery from COVID-19 and partial resolution of lymphocytosis. Thus, CLL diagnosis was confirmed, except for one case that turned into Monoclonal B lymphocytosis (MBL).
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9073957/
Importantly, cases of SARS-CoV-2 infection triggering the earlier unmasking of CLL were also reported in a Swedish study on the outcome of COVID-19 in CLL patients, where 8% (5/60) of enrolled cases were diagnosed with CLL during hospitalization. Yet, no information on lymphocytosis phenomena is available since the CLL blood count over time was not reported.
https://pubmed.ncbi.nlm.nih.gov/34564699/
Lymphocytosis is an unexpected phenomenon since it is an uncommon feature in the COVID-19 patient population, who rather tend to experience lymphopenia.
Plausible Explanations of the observed CLL B Cells Lymphocytosis during COVID-19
Typically, infections and associated inflammatory responses are believed to have a role in the pathogenesis of some CLL cases. Yet, CLL cells modulate various components of the immune system, such as T helper (Th) cells and Myeloid-Derived Suppressor Cells (MDSCs), suppressing the anti-tumor response against themselves and creating a trophic microenvironment for their own support.
The researchers say that it is possible that an immune response against SARS-CoV-2 might lead to various activations and modulations of the immune system that might be either advantageous or deleterious for the leukemic B cells.
The rather quick and high rise in the CLL cells’ blood count likely excludes (hyper)lymphocytosis due to the induced proliferation of leukemic cells. More likely, through various mechanisms evaluated below, the infection might induce outwards trafficking of CLL cells from the secondary lymphoid organs.
In most cases, peripheral CLL cells are quiescent and/or anergic, while those residing in the secondary lymphoid tissues (e.g., lymph nodes, spleen, bone marrow) compose populations of active cells responsive to stimuli and with a significant percentage of proliferating cells.
The models of in vivo kinetics of the CLL generally propose that in the secondary lymphoid organs, CLL B cells undergoing activation and/or proliferation downregulate adhesion and trafficking molecules (e.g., CXCR4) and migrate outwards.
It was noted that once in the bloodstream, they acquire less active, more quiescent/anergic phenotypes while concomitantly re-upregulating trafficking molecules.
A percentage of these CLL cells will traffic inwards toward the secondary lymphoid organs, perpetuating the cycle.
When the rates of survival/proliferation overcome those of apoptosis, CLL can progress. Hence, it is possible that during the acute phase of SARS-CoV-2 infection, part of the CLL cells residing in the secondary lymphoid tissues might undergo activation, either directly (e.g., viral antigens engaging the BCRs or TLRs of the CLL cells) or indirectly (e.g., activation of T cells and the proinflammatory response that support CLL B cells’ activation/proliferation).
All such mechanisms are known to downregulate trafficking receptors such as CXCR4 on the CLL cells, leading to outward trafficking and (hyper-)lymphocytosis.
With regards to the possible direct engagement through the BCR, CLL is known to often display polyreactive antibodies against self- and (non)self-antigens with a key role both during CLL pathogenesis and clonal evolution. Moreover, cases of CLLs expressing antibodies against bacteria or fungi identified in previous infections have been reported [17,18].
https://ashpublications.org/blood/article/111/7/3838/25079/A-new-perspective-molecular-motifs-on-oxidized-LDL
https://rupress.org/jem/article/210/1/59/41284/A-mutated-B-cell-chronic-lymphocytic-leukemia
A fraction of CLL patients might be able to express BCRs to directly react with SARS-CoV-2 antigens, therefore undergoing activation/proliferation and being released from secondary lymphoid tissues. However, this is unlikely to be the most common cause of lymphocytosis since it is observable in CLL cases expressing different antigen-binding sites.
However, direct activation of CLL cells might rather be induced through the TLR7 pathway as CLL cells are activated through the TLRs (e.g., TLR7), and RNA from SARS-CoV-2 has been found in the lymph nodes and spleen of infected individuals.
Also, CD4+ T cells are also often activated by SARS-CoV-2 infection and may show increased expression of CD40L among several activation markers.
CLL B cells require support from autologous T cells, and interaction between CD40L and CD40 might induce activation and proliferation.
Furthermore, IL-4, an important co-factor for the CD40-mediated CLL activation, is upregulated during SARS-CoV-2 infection in a significant fraction of cases. Hence, SARS-CoV-2 infection might indirectly activate CLL cells and induce the subsequent downregulation of trafficking receptors and lymphocytosis by activating the CD4+ T cells’ response against the virus.
Conversely, SARS-CoV-2-mediated activation of T cells and, more in general, of the entire immune system, might be the mechanism by which CLL cells lose the trophic niches within the secondary lymphoid organs, thus causing a passive lymphocytosis of quiescent cells, which represents a favorable process for the CLL patient.
A key question remains as to whether COVID-19 might also exacerbate underlying leukemia that is still below the clinical parameters for a positive diagnosis, as some recent reports have pointed t. As of now, it is too early to clinically evaluate a change in the CLL outcome upon COVID-19 diagnosis. Similarly, lab tests have not yet fully investigated the phenotype of CLL B cells during induced (hyper)lymphocytosis. Thus, future analyses are required to examine the activation/exhaustion of leukemic cells, helping to clarify which mechanism(s) are involved and considering possible changes in CLL therapy during and after SARS-CoV-2 infection.
For the latest
COVID-19 News, keep on logging to Thailand Medical News.