COVID-19 Research: Study Calls For Control Of Hyperglycemia In Both Diabetics And Non-Diabetics To Prevent COVID-19 Severity
Source: COVID-19 Research Aug 12, 2020 4 years, 8 months, 2 weeks, 6 hours, 53 minutes ago
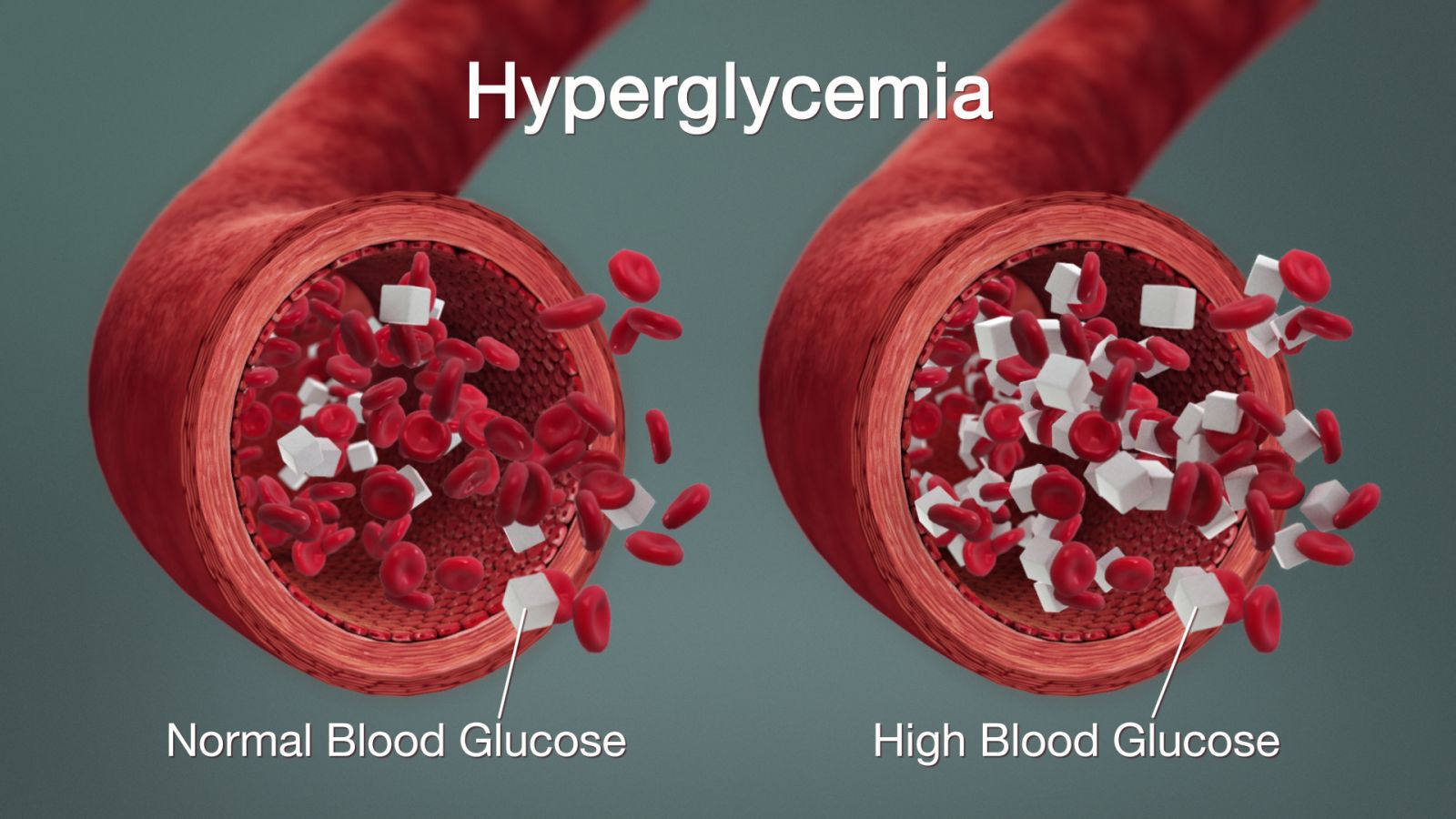
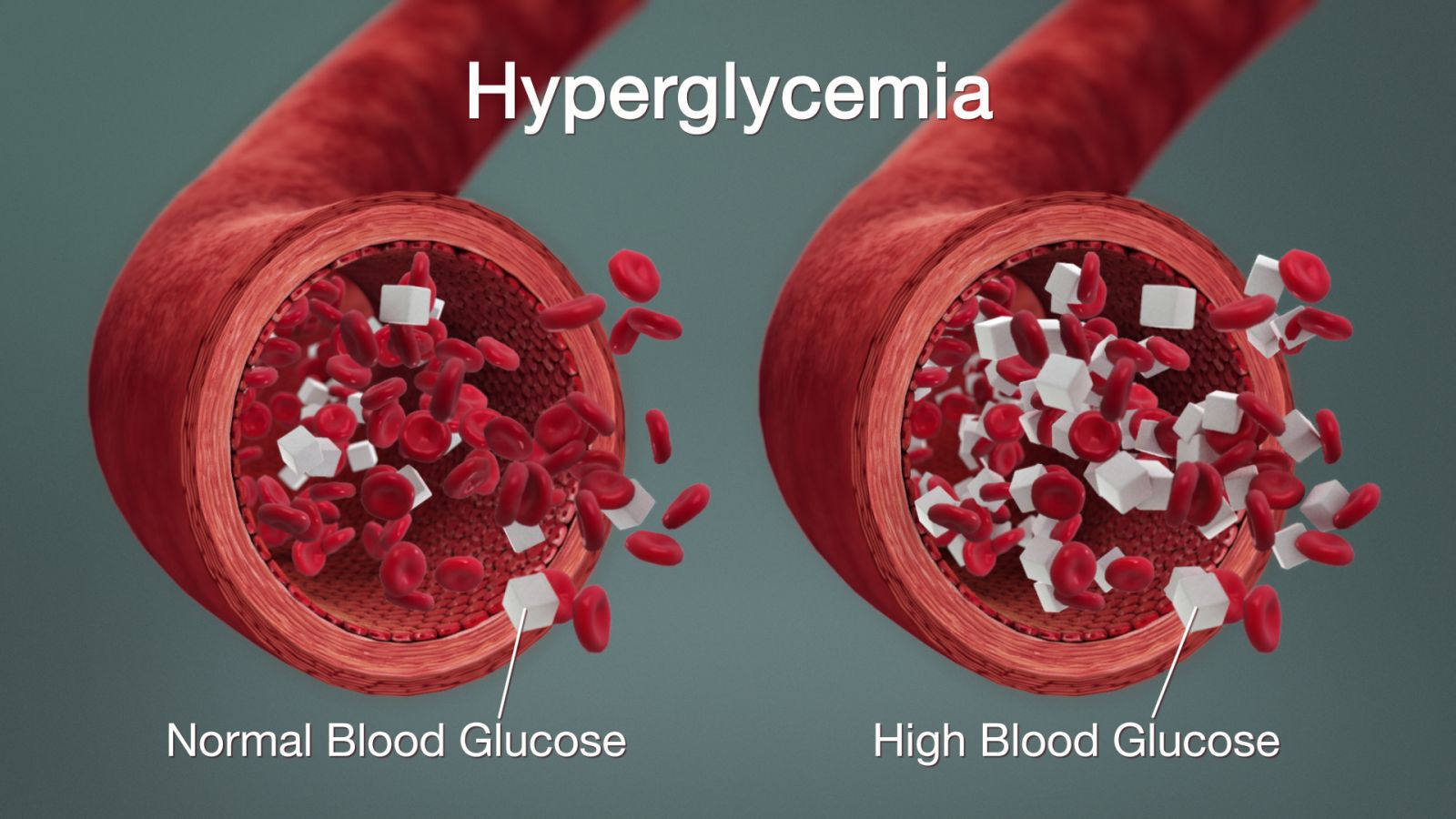
COVID-19 Research: Hyperglycemia or a condition of high blood sugar can aggravate and cause progression to severity in COVID-19 patients according to a new study by researchers from Michigan Medicine-University of Michigan. According to the researchers one of the possible explanations for this is because high sugar levels in the body triggers low inflammation which further aggravates the immunity system which is already dealing with the pathogen hence creating an ever higher ‘virus causing inflammatory reaction’. (note that the condition of hyperglycemia can also occur in non-diabetics and also those in prediabetic stages.)
The research findings were published in the journal of the American Diabetes Association: Diabetes
https://diabetes.diabetesjournals.org/content/early/2020/08/10/dbi20-0022
After a preliminary observations of 200 COVID-19 patients with severe hyperglycemia, the Michigan Medicine team’s study findings is shedding light as to why high blood sugar may trigger worse outcomes in individuals infected with the virus.
The research team have also developed a blood sugar management tool that may potentially reduce risk of secondary infections, kidney issues and intensive care stays in people with diabetes, prediabetes or obesity who get COVID-19.
First author Dr Roma Gianchandani, M.D., a Professor of Internal Medicine at the Michigan Medicine division of metabolism, endocrinology and diabetes told Thailand Medical News, "Based on preliminary observations of our patients, those with one of these pre-existing conditions are at high risk for making the virus-induced respiratory dysfunction much worse, potentially resulting in death."
Dr Rodica Pop-Busui M.D. Ph.D., the Larry. D Soderquist Professor of diabetes, Professor of internal medicine and vice chair of clinical research in the Department of Internal Medicine who is also a senior author of the study suspects it's the low grade, inflammatory nature of diabetes and hyperglycemia that promote the virus' inflammatory surge, resulting in insulin resistance and severe hyperglycemia.
.jpg)
She explained, "Typically, when the body becomes this inflamed, it triggers an abnormal immune response that instead of just attacking the virus, affects the rest of the body's healthy cells and tissue, leading to rapid deterioration in health.”
Such affected patients are at an increased risk for mechanical ventilation, kidney replacement therapy due to kidney failure and requiring medications known as vasopressors to stop dangerously low blood pressure or steroids to combat acute respiratory distress syndrome.
Dr Gianchandani adds, "All of these complications make blood sugar management more difficult, but the study team is convinced this management is essential to prevent complications that lead to prolonged inpatient stays, or morbidity."
/>
Dr Gianchandani further added, "A recent study has already shown there's a correlation between well-controlled blood sugar and lower levels of inflammatory markers."
The study team developed a tool to identify and manage high blood sugar in COVID-19 patients, placing them into certain risk categories that looked at hyperglycemia severity, presence of obesity, level of insulin resistance, extent of kidney dysfunction and evidence of rapid changes in inflammatory markers.
Implementing an algorithm
The innovative hyperglycemia management teams set out to find a way to monitor patients' diabetes without having to use more personal protective equipment to visit the rooms all the time. It was also important to reduce the health care provider's exposure to the virus as much as possible.
Despite being accurate, a continuous glucose monitor wouldn't be as helpful because a patient's low blood pressure and the use of blood pressure medications could falsely elevate blood sugar levels.
The developed treatment protocol called for insulin delivery every six hours, and at the same time a nurse would check in on the patient. Some patients who were on ventilators or receiving high doses of Vitamin C would get their arterial or venous blood sugar levels checked, replacing the need for the team's blood sugar check.
For those with the highest blood sugar levels and severe hyperglycemia, insulin infusions were an option for patients until their levels fell between a normal range.
The combined result of these efforts helped successfully lower blood sugar levels without increasing nurse contact or the overall burden on primary care teams and PPE usage.
Dr Gianchandani added, "Improving blood sugar control was important in reducing the amount of secondary infections and kidney issues this cohort of patients are susceptible to. This might help shorten ICU stays and lessen the amount of patients that need a ventilator."
The researchers say that it is important to note this algorithm was not developed as a result of a clinical trial, but is based solely on preliminary observations in the patients the team followed. A larger, randomized and controlled study is necessary to determine how this algorithm impacts mortality, time to recovery, the length of ICU stays and rate of severe complications.
Dr Gianchandani further adds, "Our study team is looking forward to the next steps in confirming our hypothesis. In the meantime, I think these observations validate the importance of blood sugar management in COVID-19 patients and can serve as a guide or inspiration for other institutions."
For the latest on
COVID-19 Research, keep on logging to Thailand Medical News.
.jpg)