COVID-19 Treatments: Study Shows Therapeutic And Prophylactic Blood Thinners Increased Survival Rates And Reduced Risk Of Intubation
Source: COVID-19 Treatments Aug 27, 2020 5 years, 3 months, 4 weeks, 11 hours, 49 minutes ago
COVID-19 Treatments: Despite an early initiative by researchers from Mount Sinai School of Medicine to show that anticoagulation therapy was associated with improved survival among hospitalized COVID-19 patients, many questions remained such as the size of the potential benefit, and about what dosage of this therapy might be more effective.
A new observational study by the same the research team has provided more perspectives and also found all regimens of anticoagulants ie drugs that prevent blood clotting were far superior to no anticoagulants in COVID-19 patients.
Significantly, it was shown that, patients on both a "therapeutic" or full dose, and those on a "prophylactic" or lower dose, showed about a 50 percent higher chance of survival, and roughly a 30 percent lower chance of intubation, than those not on anticoagulants.
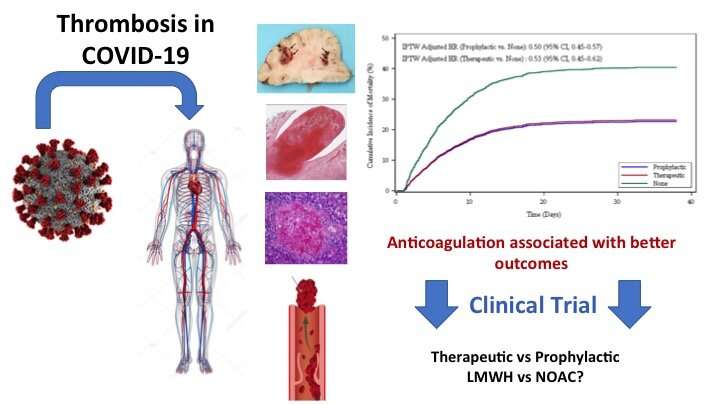
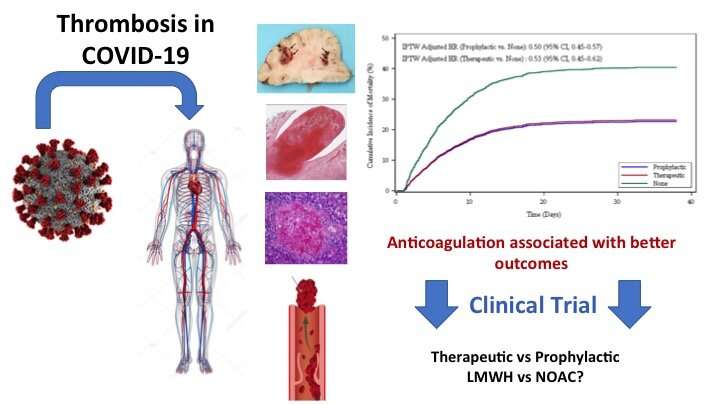 Thromboembolic disease is a complication of COVID-19. Prophylactic and therapeutic anticoagulation are associated with better outcomes in hospitalized patients with COVID-19. randomized controlled trials evaluating different AC regimens in COVID-19 are needed. Credit: Mount Sinai Health System
Thromboembolic disease is a complication of COVID-19. Prophylactic and therapeutic anticoagulation are associated with better outcomes in hospitalized patients with COVID-19. randomized controlled trials evaluating different AC regimens in COVID-19 are needed. Credit: Mount Sinai Health System
The study team assessed six different anticoagulant regimens, including both oral and intravenous dosing, within both therapeutic and prophylactic groups.
The team observed that therapeutic and prophylactic subcutaneous low-molecular weight heparin, and therapeutic oral apixaban may lead to better results.
The study findings were published in the Journal of the American College of Cardiology.
https://www.onlinejacc.org/content/76/1/122
Senior corresponding author Dr Valentin Fuster, MD, Ph.D., Director of Mount Sinai Heart and Physician-in-Chief of The Mount Sinai Hospital and one of the world’s leading researcher in the field of cardiology and cardiovascular issues told Thailand Medical News, "This work from the Mount Sinai COVID Informatics Center provides additional insight on the role of anticoagulation in the management of patients admitted to the hospital with COVID-19. Although this is an observational study, it helped in the design of a large-scale international clinical trial that we are coordinating. The randomized trial focuses on those three antithrombotic regimens ie therapeutic and prophylactic subcutaneous low-molecular weight heparin, and therapeutic oral apixaban.”
This new observational study is an extension of Mount Sinai research that showed that treatment with anticoagulants was associated with improved outcomes both in and out of the intensive care unit among hospitalized COVID-19 patients. The work was prompted by the discovery that many patients hospitalized with COVID-19 developed high levels of life-threatening blood clots.
The study team evaluated electronic medical records of 4,389 confirmed COVID-19-positive patients admitted to five hospitals in the Mount Sinai Health System in New York City (The Mount Sinai
Hospital, Mount Sinai West, Mount Sinai Morningside, Mount Sinai Queens, and Mount Sinai Brooklyn) between March 1 and April 30, 2020. They specifically looked at survival and death rates for patients placed on therapeutic and prophylactic doses of blood thinners (oral antithrombotics, subcutaneous heparin, and intravenous heparin) versus those not placed on blood thinners.
The team used a hazard score to estimate risk of death, which took relevant risk factors into account before evaluating the effectiveness of anticoagulation, including age, ethnicity, pre-existing conditions, and whether the patient was already on blood thinners. The researchers also took into account and corrected for disease severity, including low oxygen saturation levels and intubation.
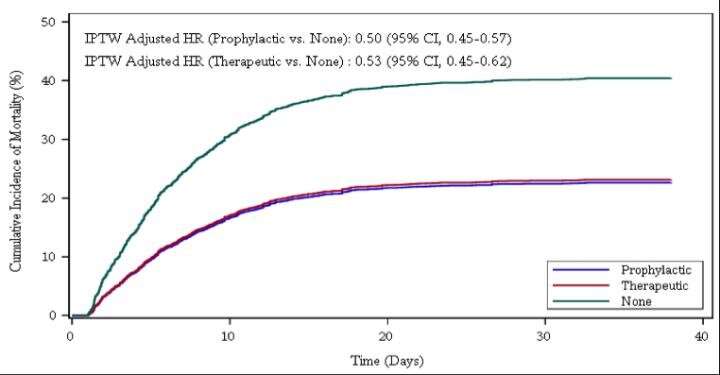
From the total patients analyzed, 900 (20.5 percent) received a full-treatment dose of anticoagulants. Another 1,959 patients (44.6 percent) received a lower, prophylactic dose of anticoagulants, and 1,530 (34.5 percent) were not given blood thinners. There was a strong association between blood thinners and reduced likelihood of in-hospital deaths: both therapeutic and prophylactic doses of anticoagulants reduced mortality by roughly 50 percent compared to patients on no blood thinners.
Interestingly, on the whole 467 (10.6 percent) of the patients required intubation and mechanical ventilation during their hospitalization. Those on therapeutic blood thinners had 31 percent fewer intubations than those not on blood thinners, while those on prophylactic blood thinners had 28 percent fewer.
It was also surprising to observe that bleeding rates - a known complication of blood thinners were surprisingly low overall among all patients (three percent or less), but slightly higher in the therapeutic group compared to the prophylactic and no-blood-thinner groups, the researchers said. Their findings suggest that clinicians should evaluate patients on an individual basis given the benefit-risk tradeoff.
The study team also looked at autopsy results of 26 COVID-19 patients and found that 11 of them (42 percent) had blood clots—pulmonary, brain, and/or heart that were never suspected in the clinical setting. These findings suggest that treating patients with anticoagulants may be associated with improved survival.
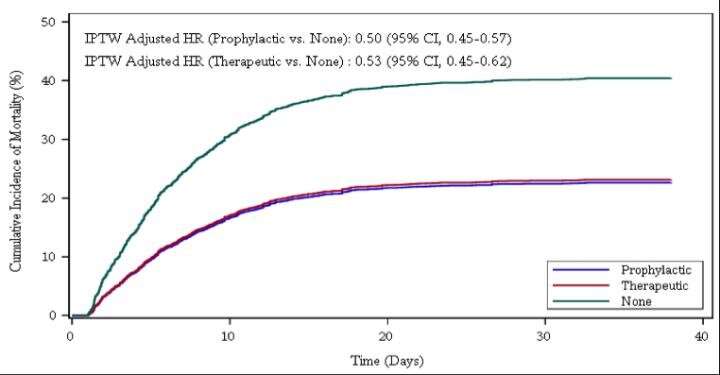 Stabilized weight adjusted cumulative incidence curves for the effect of anticoagulation on in-hospital mortality with discharge as a competing risk. The estimates are adjusted for the invers probability of treatment weighting (IPTW) using propensity scores. Hazard ratio (HR) and 95% confidence interval (CI) are based on stabilized IPTW Fine and Gray's sub-distribution hazard models with robust variance and discharge as a competing event. The multivariable model includes therapeutic and prophylactic anticoagulation as time-dependent variables and controls for the effect of time-varying intubation status and respiratory rate and oxygen saturation at admission. Stabilized weight adjusted cumulative incidence curves for the effect of anticoagulation on intubation with death and discharge as competing risks. The estimates are adjusted for the inverse probability of treatment weighting (IPTW) using propensity scores. Hazard ratio (HR) and 95% confidence interval (CI) are based on stabilized IPTW Fine and Gray's sub-distribution hazard models with robust variance and death and discharge as competing events. The multivariable model includes therapeutic and prophylactic anticoagulation as time-dependent variables and controls for the effect of respiratory rate and oxygen saturation at admission. Credit: Mount Sinai Health System
Stabilized weight adjusted cumulative incidence curves for the effect of anticoagulation on in-hospital mortality with discharge as a competing risk. The estimates are adjusted for the invers probability of treatment weighting (IPTW) using propensity scores. Hazard ratio (HR) and 95% confidence interval (CI) are based on stabilized IPTW Fine and Gray's sub-distribution hazard models with robust variance and discharge as a competing event. The multivariable model includes therapeutic and prophylactic anticoagulation as time-dependent variables and controls for the effect of time-varying intubation status and respiratory rate and oxygen saturation at admission. Stabilized weight adjusted cumulative incidence curves for the effect of anticoagulation on intubation with death and discharge as competing risks. The estimates are adjusted for the inverse probability of treatment weighting (IPTW) using propensity scores. Hazard ratio (HR) and 95% confidence interval (CI) are based on stabilized IPTW Fine and Gray's sub-distribution hazard models with robust variance and death and discharge as competing events. The multivariable model includes therapeutic and prophylactic anticoagulation as time-dependent variables and controls for the effect of respiratory rate and oxygen saturation at admission. Credit: Mount Sinai Health System
Corresponding author Dr Anu Lala, MD, Assistant Professor of Medicine (Cardiology) and Director of Heart Failure Research at the Icahn School of Medicine at Mount Sinai added, "This report is much more in-depth than our previous brief report and includes many more patients, longer follow-up, and rigorous methodology. Clearly, anticoagulation is associated with improved outcomes and bleeding rates appear to be low. As a clinician who has treated COVID-19 patients on the front lines, I recognize the importance of having answers as to what the best treatment for these patients entails, and these results will inform the design of clinical trials to ultimately give concrete information."
First author Dr Girish Nadkarni, MD, Co-Founder and Co-Director of the Mount Sinai COVID Informatics Center and Clinical Director of the Hasso Plattner Institute for Digital Health at Mount Sinai said, “These observational analyses were done with the highest level of statistical rigor and provide exciting insights into the association of anticoagulation with critical in-hospital outcomes of mortality and intubation. We are excited that results from this observational study in one of the largest and most diverse hospitalized populations have led to an ongoing trial of type, duration, and doses of anticoagulation. Ultimately we hope this work will lead to improved outcomes and treatment for COVID-19 patients."
Co-author Dr Zahi Fayad, Ph.D., Co-Founder of the Mount Sinai COVID Informatics Center and Director of Mount Sinai's BioMedical Engineering and Imaging Institute added, "This work highlights the need to better understand the disease from a diagnostic and therapeutic point of view and the importance of conducting properly designed diagnostic and interventional studies.”
For more about
COVID-19 Treatments, keep on logging to Thailand Medical New