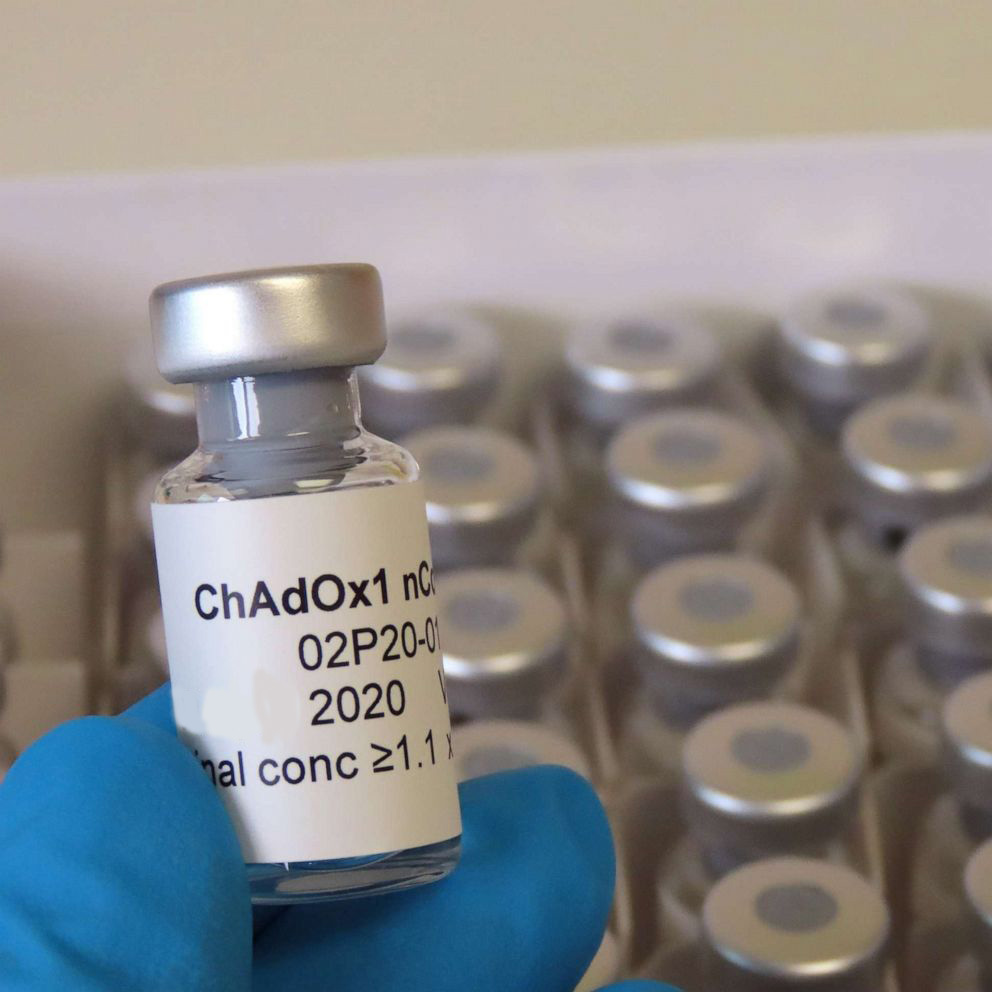
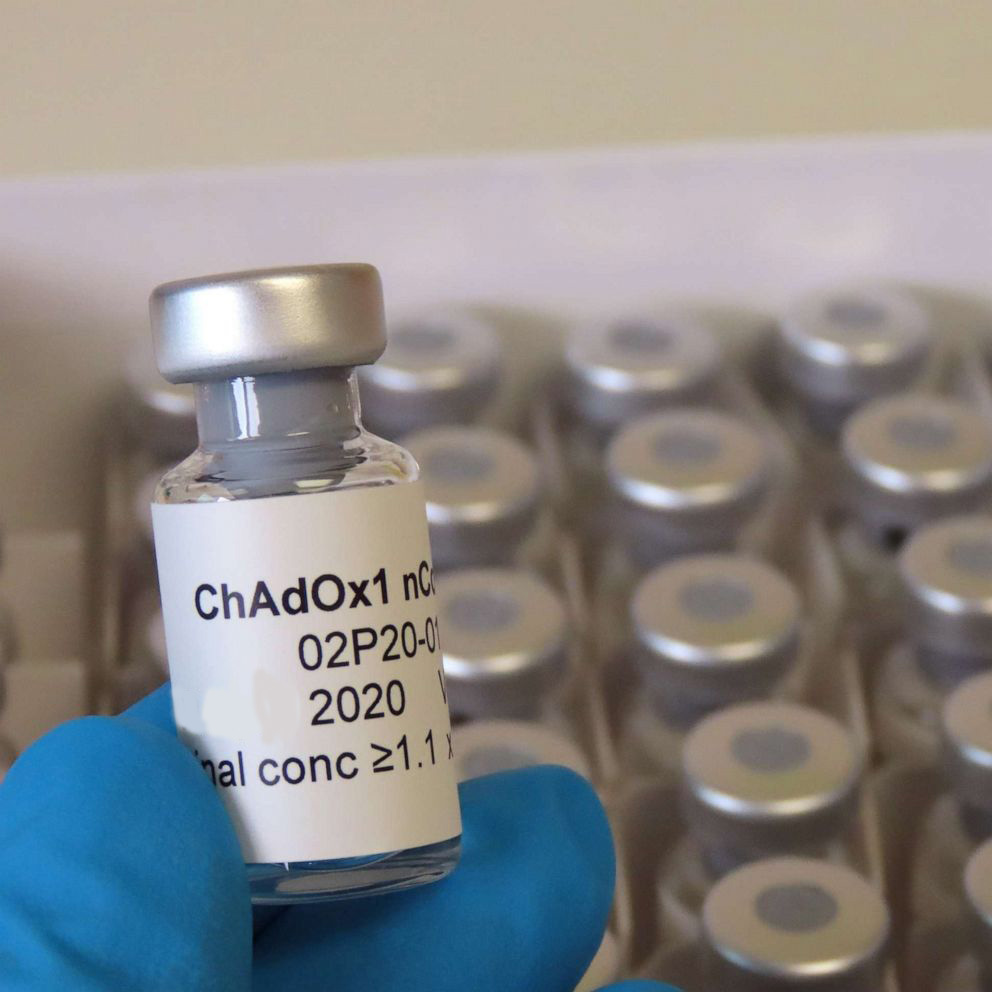
COVID-19 Vaccine: Oxford’s and AstraZenaca’s ChAdOx1 Vaccine Progresses Into Phase III Human Trials
Source: COVID-19 Vaccine Jul 06, 2020 4 years, 9 months, 2 weeks, 6 days, 15 hours, 31 minutes ago
COVID-19 Vaccine: Professor of vaccinology at the University of Oxford, and one of the scientists leading the vaccine initiative, Dr Sarah Gilbert, told the U.K.'s Science and Technology Committee last week that their candidate vaccine has progressed to the phase III trial in the United Kingdom.
Phase III trials typically involves tens of thousands of research participants across various countries in order to show a statistically significant difference.
The vaccine technically named ChAdOx1 nCoV-19 (AZD1222) is made from a virus called ChAdOx1, which is a weakened and non-replicating version of a common cold virus (adenovirus). The vaccine has been engineered to express the SARS-CoV-2 spike protein.
This phase III trial will involve testing the candidate vaccine in approximately 8,000 people in the United Kingdom. The researchers have also given the vaccine to a few hundred people in Brazil, but over the next couple of weeks, the number may increase to about 5,000 people. The team also plans to trial the vaccine for 2,000 people in South Africa.
The ChAdOx1 vaccine, AZD1222, which is licensed to AstraZeneca, has been shown to trigger an immune response against SARS-CoV-2. Though the researchers believe the results are promising, they cannot give a specific timeframe on when it can be ready for public use.
The study team said that the candidate vaccine was created with the use of the ChAdOx1 vaccine technology, which was based on an adenovirus. This virus causes mild upper respiratory tract infections. They removed some parts of the viral genes to develop it as a vaccine. It is considered safe even in people with a weak immune system.
The ChAdOx1 vaccine was made by adding genetic material called spike glycoprotein that is expressed on the surface of SARS-CoV-2 to the ChAdOx1 virus. This spike glycoprotein is usually found on the surface of the novel coronavirus and is what gives the coronavirus its distinct spiky appearance. These spikes play an essential role in laying a path for infection by the coronavirus. The virus that causes Covid-19 uses this spike protein to bind to ACE2 receptors on human cells.
The study team have shown that antibodies produced against sections of the spike protein after natural infection are able to neutralize (kill) the virus when tested in the laboratory.
The scientist, by vaccinating volunteers with ChAdOx1 nCoV-19, hope to make the human body recognize and develop an immune response (i.e., develop antibodies) to the spike glycoprotein that will help stop the SARS-CoV-2 virus from entering human cells and causing COVID-19.
This biotechnology has been used to produce candidate vaccines against other pathogens, such as those causing flu, Zika infection, Chikungunya, and another coronavirus, the Middle East Respiratory Syndrome (MERS).
Professor Dr Sarah Gilbert, who is leading the University of Oxford, told Thailand Medical News, "Vaccines have a different way of engaging with the immune system, and we follow people in our studies using the same type of technology to make the vaccines for several years, and we still see strong immune responses."
She further added, "It is something we have to test and follow over time we can'
;t know until we have the data but we're optimistic based on earlier studies that we will see a good duration of immunity, for several years at least, and probably better than naturally-acquired immunity.”
Some experts however fear that vaccines might not offer long-term protection against the novel coronavirus, given that those with other types of coronavirus, such as the common cold, had been re-infected with a year.
A study from the Oxford UK vaccine research group revealed that a single dose of ChAdOx1 nCoV-19 (AZD1222) induces antigen-specific antibody and T cells responses against the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), and a booster shot additionally enhanced antibody production with an increase in neutralizing titers particularly in pigs.
https://www.biorxiv.org/content/10.1101/2020.06.20.159715v1
Professor Dr Simon P. Graham, the corresponding author of that study who is from Pirbright Institute-UK said, "A single dose of ChAdOx1 nCoV-19 induces antibody responses, but we demonstrate here that antibody responses are significantly enhanced after a homologous boost in one mouse strain and to a greater extent in pigs.”
The competition to develop a vaccine will intensify as the northern hemisphere nears the winter season when the cases are expected to rise. The Oxford vaccine scientists, however, hope that the vaccine may be ready by early 2021.
The research team hopes it could be earlier but could not specify the exact timeline since it will rely on the results of the trial.
The team has gained immense focus from across the globe with its positive preliminary results. In June, AstraZeneca announced that it had won a $1.2 billion contract with the United States government to produce about 400 million doses of the candidate vaccine once it becomes ready. Further, the firm also signed a contract with the British government to produce up to 100 million doses, adding that 30 million may be ready for citizens in the U.K. by September.
Despite all the optimism, many experts are warning that these vaccines will only be able to offer short-term protection for not more than 2 months or so and that with the SARS-CoV-2 coronavirus still evolving smartly but slowly, there will be surprises to show that most of these efforts and money spent will be in vain.
For more on
COVID-19 vaccines, keep on logging to Thailand Medical News.