COVID-19 Vaccines Causes Persistence Of Spike Protein In The CD16+ Monocytes And Makes SARS-CoV-2 Negative People Sick With PASC-Like Sickness!
Nikhil Prasad Fact checked by:Thailand Medical News Team Mar 27, 2024 1 year, 8 months, 2 weeks, 3 days, 3 hours, 52 minutes ago
Spike Protein Found In CD16+ Monocytes Up To 245 Days In The COVID-19 Vaccinated Who Were SARS-CoV-2 Negative But Had Long-COVID-Like Symptoms!
COVID-19 News: In recent times, the global focus on combating the COVID-19 pandemic has been primarily directed towards vaccination efforts. With billions of doses administered worldwide, vaccines such as BNT162b2 (Pfizer), mRNA-1273 (Moderna), Janssen (Johnson and Johnson), and ChAdOx1 nCoV-19 (AstraZeneca) have been claimed to have played a pivotal role in reducing severe illness and mortality associated with SARS-CoV-2 infection although there seem to be detailed and accurate data that shows as such.
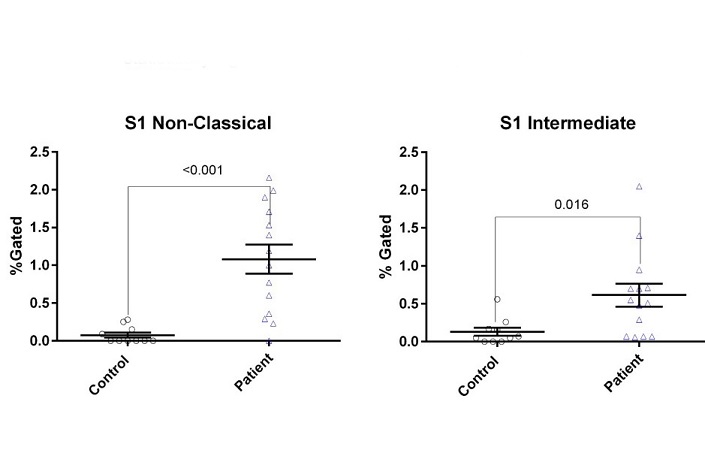
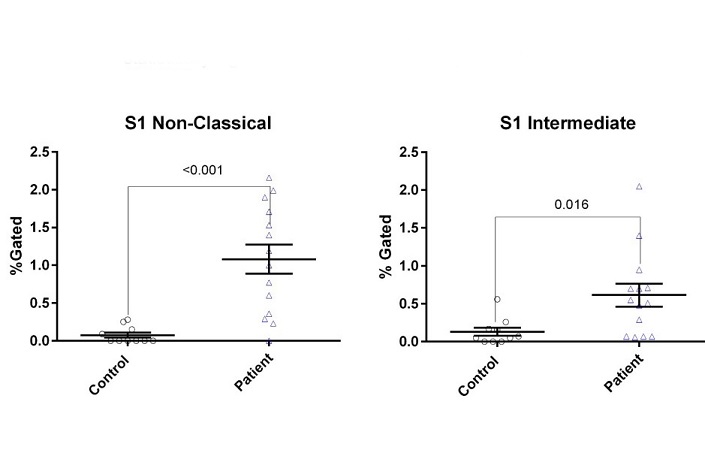 S1 Spike Protein Found In CD16+ Monocytes Up To 245 Days In The COVID-19 Vaccinated Who Were SARS-CoV-2 Negative But Had Long-COVID-Like Symptoms! Flow cytometric quantification of S1-containing monocyte subsets as previously performed. Increased S1-conatining intermediate and non-classical monocytes was statistically significant compared to healthy controls.
S1 Spike Protein Found In CD16+ Monocytes Up To 245 Days In The COVID-19 Vaccinated Who Were SARS-CoV-2 Negative But Had Long-COVID-Like Symptoms! Flow cytometric quantification of S1-containing monocyte subsets as previously performed. Increased S1-conatining intermediate and non-classical monocytes was statistically significant compared to healthy controls.
However, alongside the claimed “success” of vaccination campaigns, there have been reports of individuals experiencing persistent symptoms reminiscent of Post-Acute Sequelae of COVID-19 (PASC) or long COVID despite being SARS-CoV-2 negative.
This
COVID-19 News report delves into a study conducted by researchers from IncellDx Inc, California, Lawrence General Hospital-Massachusetts, Francis Medical Center, New Jersey,Novant Health Kernersville Medical Center, North Carolina, New York Presbyterian Hospital, Brooklyn, Stamford Hospital, Connecticut, Marshfield Medical Center, Wisconsin and Universidad de Costa Rica, that investigated the presence of SARS-CoV-2 S1 spike protein in CD16+ monocytes of individuals who received COVID-19 vaccination but exhibited PASC-like symptoms. The study aimed to shed light on the immunologic abnormalities contributing to these symptoms and explore potential similarities with PASC.
Background and Objectives
The emergence of PASC, characterized by persistent symptoms lasting beyond 30 days post-COVID-19 infection, raised concerns regarding similar prolonged effects post-vaccination. The objective of this study was to analyze the immune profiles of individuals experiencing new-onset PASC-like symptoms after COVID-19 vaccination and to investigate the presence of SARS-CoV-2 S1 spike protein in CD16+ monocytes as a possible etiological factor.
Methodology
The study involved 50 individuals with post-vaccination PASC-like symptoms and 45 vaccinated individuals without such symptoms as controls. Multiplex cytokine/chemokine profiling and machine learning techniques were employed to analyze immune profiles. Flow cytometry and
mass spectrometry were utilized to detect SARS-CoV-2 S1 protein in CD16+ monocyte subsets.
Results
The average age of individuals with PASC-like symptoms was 41.8 years, with a predominant female representation. Symptoms such as fatigue, neuropathy, brain fog, and headache were common among these individuals, irrespective of the vaccine received.
Immune profiling revealed significant elevations in cytokines/chemokines such as sCD40L, CCL5, IL-6, and IL-8 in post-vaccination individuals with PASC-like symptoms compared to controls.
Analysis of S1 protein persistence in CD16+ monocytes showed statistically significant elevations in S1-containing non-classical and intermediate monocytes among individuals with PASC-like symptoms post-vaccination.
Post-COVID vaccination individuals with PASC-like symptoms exhibit markers of platelet activation and pro-inflammatory cytokine production, which may be driven by the persistence of SARS-CoV-2 S1 proteins in intermediate and non-classical monocytes
The average days from last inoculation with a COVID vaccine and time of blood draw for this study was 105 days. The greatest time period from inoculation to blood draw was 245 days and the shortest time period was 38 days. 27 individuals reported receiving BNT162b2 (Pfizer), 15 received mRNA-1273 (Moderna), 7 received Janssen (Johnson and Johnson), and 1 individual received ChAdOx1 nCoV-19 (AstraZeneca) vaccine.
Discussion
The study findings suggest a potential link between persistent S1 protein in CD16+ monocytes and post-vaccination PASC-like symptoms. Elevated cytokine levels indicative of inflammation were observed in these individuals, resembling patterns seen in PASC patients. The presence of S1 protein in monocytes raises questions about the pathophysiology of prolonged symptoms post-vaccination.
Thailand
Medical News had also covered another study a few days ago that showed that the lipids in the COVID-19 mRNA vaccines induced complement activation and inflammatory issues that were similar to actual SARS-CoV-2 infections!
https://www.thailandmedical.news/news/breaking-mrna-lnp-covid-19-vaccine-lipids-induce-complement-activation-and-adverse-proinflammatory-issues-similar-to-actual-infections
Limitations
One major limitation of the study is the lack of approved testing to definitively rule out previous SARS-CoV-2 infection, which could confound the results regarding S1 protein persistence. Additionally, the study does not provide epidemiological insights into the prevalence of post-vaccination PASC-like symptoms.
Implications
The study's findings contribute to ongoing discussions about vaccine safety and efficacy, urging healthcare professionals and policymakers to consider potential long-term effects post-vaccination.
The study highlights the need for further research to understand the risk factors, prevalence, and mechanisms underlying persistent post-vaccination symptoms. It also emphasizes the importance of developing targeted therapies based on immunologic abnormalities identified in affected individuals.
Conclusion
In conclusion, the persistence of SARS-CoV-2 S1 spike protein in CD16+ monocytes post-vaccination raises intriguing questions about the etiology of PASC-like symptoms in vaccinated individuals. This study underscores the complexities of immune responses following vaccination and emphasizes the need for comprehensive monitoring and research to address emerging challenges in post-vaccine complications. Further investigations are warranted to validate these findings and inform clinical management strategies for affected individuals.
The study findings were published on a preprint server and is currently being peer reviewed.
https://www.medrxiv.org/content/10.1101/2024.03.24.24304286v1
For the latest
COVID-19 News, keep on logging to Thailand Medical News.