Nikhil Prasad Fact checked by:Thailand Medical News Team May 15, 2024 1 year, 7 months, 2 weeks, 6 days, 14 hours, 44 minutes ago
COVID-19 News: In the shadow of the global COVID-19 pandemic, a new and troubling health issue has come to light: COVID-19 related osteonecrosis of the jaws (CRONJ). Dental researchers from the Faculty of Dentistry at the University of São Paulo in Brazil and Mashhad Dental School at Mashhad University of Medical Sciences in Iran have reported cases that underline this emerging condition. These cases which are covered in this
COVID-19 News report, which were treated at Imam Reza Hospital in Mashhad, Iran, reveal a disturbing link between severe COVID-19 and the onset of jaw osteonecrosis, highlighting the need for increased vigilance among healthcare professionals.
 Dental Researchers Warn That COVID-19 Can Also Cause
Dental Researchers Warn That COVID-19 Can Also Cause
Osteonecrosis Of The Jaws!
Osteonecrosis also known as avascular necrosis is basically bone death caused by poor blood supply. It is most common in the hip and shoulder but can affect other large joints such as the knee, elbow, wrist, and ankle.
Thailand
Medical News had already previously covered a study in which it was found that about six percent of post-COVID individuals are likely to suffer from hip issues due to necrosis of the femoral head caused by SARS-CoV-2 infection.
https://www.thailandmedical.news/news/six-percent-of-all-post-covid-patients-who-have-hip-discomfort-likely-to-have-developed-avascular-necrosis-of-the-femoral-head
A New Aftermath of COVID-19: The Silent Threat
The COVID-19 pandemic has left an indelible mark on global health, with millions affected by the virus in varying degrees of severity. While the immediate impacts of COVID-19 are well-documented, the long-term consequences are still being uncovered. Among these is the emerging condition of CRONJ, which has only recently been identified by medical professionals. This condition, characterized by the death of jawbone tissue, has added another layer of complexity to the already multifaceted aftermath of COVID-19.
In a retrospective study, two patients with suspected CRONJ were admitted to Imam Reza Hospital. These cases provide critical insights into the manifestation and potential treatments for this condition. One patient unfortunately fled the hospital before receiving treatment, while the other showed significant improvement following the proposed intervention.
Case Studies: Unmasking CRONJ
Case 1: A Missed Opportunity
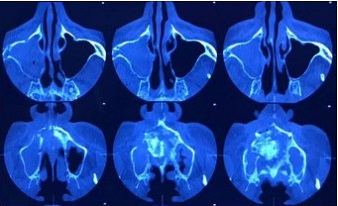
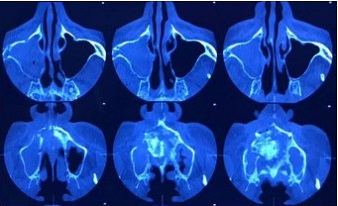
A 46-year-old male patient from Iraq presented with severe pain in the maxillofacial region, specifically in the right mid-face. Despite denying any history of trauma or chronic illness and not being on any long-term medication, he exhibite
d symptoms of osteonecrosis. His intraoral examination revealed exposed bone in the right maxillary premolar area, with a necrotic appearance and a putrid odor, suggesting chronic osteomyelitis with focal abscess formation. Further investigation uncovered that he had contracted COVID-19 six months prior and had been treated with hydroxychloroquine and high-dose dexamethasone for two months.
Given his medical history, CRONJ was suspected. The medical team recommended exploratory surgery and local debridement to remove necrotic bone tissue and promote revascularization. However, the patient, disagreeing with the treatment plan, left the hospital without undergoing the procedure.
Case 2: A Path to Recovery
A 40-year-old female patient from Iran also presented with severe maxillofacial pain. Her physical examination revealed bone exposure in the maxillary right premolar area. Similar to the first case, she had no history of trauma or chronic illness and was not on long-term medication. However, she had been hospitalized for three months due to severe COVID-19 and had received high doses of corticosteroids along with antibiotics like imipenem, colistin, and meropenem.
A local biopsy confirmed osteomyelitis without fungal involvement, leading to a diagnosis of CRONJ. The patient consented to the proposed treatment involving sequestrectomy and revascularization under local anesthesia. The procedure included the removal of six teeth and the use of platelet-rich fibrin (PRF) to enhance healing. Following the surgery, the patient was symptom-free and under regular follow-up, awaiting full recovery and potential prosthetic rehabilitation.
The Broader Implications: Understanding and Addressing CRONJ
The reports from Mashhad are not isolated incidents. Similar cases have been documented globally, with occurrences noted in the United States, Bulgaria, Uzbekistan, and Egypt. These reports share common threads: severe COVID-19 infection, hospitalization, and the use of high-dose corticosteroids.
The Role of Corticosteroids and Other Medications
Corticosteroids, a cornerstone in managing severe COVID-19, particularly for pulmonary damage, have been identified as a significant risk factor for osteonecrosis. Their prolonged use disrupts bone homeostasis by affecting osteoblast and osteoclast function and altering mineral metabolism. This disruption can lead to osteonecrosis and osteoporosis. Other medications used in COVID-19 treatment, such as tocilizumab and denosumab, have also been linked to medication-related osteonecrosis of the jaws (MRONJ).
Diagnostic Challenges and Recommendations
Diagnosing CRONJ involves differentiating it from other conditions like MRONJ, osteoradionecrosis, and osteomyelitis. Prompt investigation of symptoms, especially joint pain, is crucial. Recommended diagnostic tests include blood calcium, phosphate, vitamin D levels, parathyroid hormone, blood count, and bone mineral density assessments. Increasing daily intake of calcium and vitamin D may also help mitigate risk.
Treatment Strategies: From Surgery to Conservative Management
Treatment of CRONJ varies depending on the severity of the condition. For aggressive cases, sequestrectomy - removal of necrotic bone - is the treatment of choice to prevent the spread of osteonecrosis. Conservative approaches, such as local cleaning, antibiotics, and regular debridement, may suffice for milder cases. The use of adjunctive therapies like PRF can enhance healing and outcomes.
Looking Forward: The Need for Further Research
The current understanding of CRONJ is still evolving, and there is a clear need for further research. Larger, randomized clinical trials are necessary to evaluate the effectiveness of various treatments and to better understand the pathophysiology of CRONJ. The limited number of reported cases underscores the importance of continued vigilance and investigation.
Conclusion: Vigilance and Preparedness in the Post-COVID Era
As the world continues to grapple with the long-term effects of COVID-19, healthcare professionals must remain vigilant for emerging conditions like CRONJ. Maxillofacial and orthopedic surgeons, in particular, should consider CRONJ in their differential diagnoses for patients with a history of severe COVID-19, especially those who have received high-dose corticosteroids.
These cases studies provide valuable insights into the presentation and treatment of CRONJ. They also highlight the importance of patient compliance and the challenges of managing new and complex conditions in the post-COVID landscape. By staying informed and prepared, the medical community can better navigate these challenges and improve outcomes for patients affected by this new aftermath of the pandemic.
The study and cases reports were published in the peer reviewed World Journal of Plastic Surgery.
https://wjps.ir/article-1-1220-en.html
For the latest
COVID-19 News, keep on logging to Thailand
Medical News.