Diets And Nutrition: Italian Review Says Keto Diet Could Help To Prevent And Mitigate COVID-19 Severity
Source: Diets And Nutrition Nov 30, 2020 5 years, 1 month, 2 weeks, 4 days, 20 hours, 32 minutes ago
Diets And Nutrition: A new review published in the Journal of Translational Medicine by Italian researchers from the University of Padua- Italy and IRCCS San Raffaele Pisana-Rome-Italy says that Keto diets could help to prevent and mitigate COVID-19 severity.
https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-020-02600-9
Thailand Medical News had also published earlier in September another study by researchers from Yale School of Medicine, New York University and Washington University School of Medicine that Keto diets could help elderly COVID-19 patients.
https://www.thailandmedical.news/news/ketogenic-diet-and-covid-19-yale-led-study-advocates-keto-diet-for-elderly-covid-19-patients-due-to-possible-benefits-and-better-clinical-outcomes
The COVID-19) disease is posing a serious challenge to the health-care systems worldwide, with an enormous impact on health conditions and loss of lives. Notably, obesity and its related comorbidities are strictly related with worse clinical outcomes of COVID-19 disease. Recently, there is a growing interest in the clinical use of ketogenic diets (KDs), particularly in the context of severe obesity with related metabolic complications. KDs have been proven effective for a rapid reduction of fat mass, preserving lean mass and providing an adequate nutritional status. In particular, the physiological increase in plasma levels of ketone bodies exerts important anti-inflammatory and immunomodulating effects, which may reveal as precious tools to prevent infection and potential adverse outcomes of COVID-19 disease.
The Italian researchers here discuss the importance of KDs for a rapid reduction of several critical risk factors for COVID-19, such as obesity, type 2 diabetes and hypertension, based on the known effects of ketone bodies on inflammation, immunity, metabolic profile and cardiovascular function. We do believe that a rapid reduction of all modifiable risk factors, especially obesity with its metabolic complications, should be a pillar of public health policies and interventions, in view of future waves of SARS-CoV-2 infection.
To date there is much evidence that obesity, hypertension and cardiovascular disease contribute significantly to adverse outcomes following COVID-19 infcetion. It is rational to apply the principles of primary prevention in the attempt to contain this pandemic, by mitigating these risk factors.
Ketogenic diets (KD) may be useful in this area, with its track history of effectual reduction of fat mass, anti-inflammatory and immunomodulatory effects, and consequent improvement of cardiovascular health.
The COVId-19 pandemic caused by the SARS-CoV-2) virus is unique in that the virus is not an especially lethal pathogen, compared to Ebola, SARS, MERS or Lassa fever, with an overall case fatality ratio of 2.3%. However, it has led to the global imposition of lockdown measures, because of the rapid spread of the virus. Since this leads to thousands of new infections every day, even this small proportion of critical infection rapidly
causes hospitals and intensive care units to fill up with patients requiring constant and multidisciplinary care. The outcome is that many patients are denied care, in the worst-case scenario as happened in Italy, while the healthcare system undergoes massive overwhelm, both due to overwork and the fact that many healthcare workers are infected or even die.
Although obesity and cardiovascular risk factors predispose towards a poorer outcome, it is also important to note that the lockdown period in many cases led to a more sedentary lifestyle, which in itself may have worsened the health conditions of society as a whole. This results from insulin resistance, increased fat deposition, and low-grade inflammation, associated with obesity. Such individuals show an overall poor metabolic profile.
Typically the state of sarcopenic obesity is a combination of poor muscle mass with high fatty tissue mass, and involves poor nutrition, reduced antiviral immunity, as well as dysregulated metabolism and inflammatory pathways. The authors note that this state in patients with critical COVID-19 is more commonly associated with a poor outcome than obesity without sarcopenia.
Also, obesity is known to shift the individual to a high-risk COVID-19 group at a relatively younger age.
Importantly this relationship could be explained by the effect of fat deposition on the vertical movement of the diaphragm, restricting the lung capacity, as well as the immune and metabolic effects, and the low-grade inflammation induced by obesity. Fat cells also express ACE at high levels, which might indicate that the virus is harbored within these cells and that they act strategically to magnify the cytokine cascade to dangerous or dysregulated levels.
It was found that dietary interventions are important in reducing this risk, most importantly by restricting junk food consumption, while substituting foods with high antioxidant and anti-inflammatory properties. Such lifestyle interventions are all the more crucial in view of the fact that several pharmacological therapies for diabetes or hypertension also play a key role in the homeostasis of glucose – in inflammation, and in renal activity as well as in cardiovascular health.
For example, dipeptidyl peptidase-4 (DPP-4) inhibitors are used to lower glucose levels and influence the activity of many immunomodulatory molecules. ACE2 is the most widely recognized SARS-CoV-2 receptor in human host cells, and in mouse models, it has been found to be present at higher levels in the tissues of diabetic mice, though corresponding findings in humans are not available. Though this does not warrant discontinuation of such drugs as angiotensin receptor blockers (ARBs) or ACE inhibitors, two important anti-hypertensive classes, the authors say, "The possibility to avoid or interrupt potentially harmful pharmacological therapies with a lifestyle intervention should be carefully taken into consideration."
Individuals with diabetes are more prone to acute viral respiratory infections such as H1N1 influenza, and high glucose levels have an immunosuppressive effect. Chinese research suggests a higher mortality associated with high plasma glucose levels in COVID-19 patients, which agrees with earlier studies in H1N1 and SARS patients.
Individuals with diabetes appear to have poor lung function, thickening of the vascular membrane and alveolar epithelium, and an increased risk of acute respiratory distress syndrome (ARDS) is associated with a high glucose level at admission. The high glucose levels may also affect the immune and inflammatory pathways that drive the pathogenesis of pneumonia in these individuals. This may also increase the levels of glycosylated virus and glycosylated receptors, perhaps boosting up the susceptibility to the virus or to the severity of the illness.
Past research have shown a link between hyperglycemia and high glucose concentrations in lung tissue, which, in turn, promotes infection and replication of the flu virus. In fact, with SARS-CoV-2, the virus is known to increase the production of reactive oxygen species (ROS), which, through a chain of processes, favors highly glycolytic metabolism of monocytes and macrophages, thus increasing the rate of replication markedly. The authors suggest that inhibitors of aerobic glycolysis could correct metabolism and thus suppress viral replication.
Also it was found that dysregulated inflammation also plays a major role in severe COVID-19, initiated by a delayed interferon-gamma response, with a lymphopenic state and prolonged inflammation. Hyperglycemia is a known immunosuppressant and pro-inflammatory state, with diabetics showing high M1 macrophages and low NK cell activity. In addition, they have a Th1/Th2 imbalance, with Th17 cells predominating over Treg cells.
This low-grade inflammation that accompanies excessive adipose tissue deposition is due to gut-derived dietary metabolites, fat cell-derived factors and cytokines related to cell death. These signals are amplified by recruited monocytes and macrophages that remove cell debris. Many inflammatory markers are correlated with the percentage of fat in the body, supporting the existence of this connection.
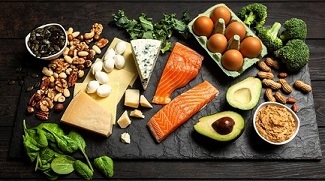
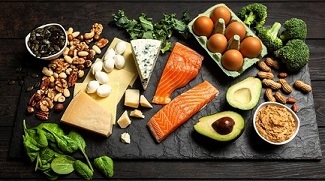
Typically ketogenic diets (KDs) are a lifestyle intervention that aims at changing the metabolic state in the host from one that utilizes primarily carbohydrates to ketone-based metabolism, by a high-fat, low-carbohydrate dietary pattern. Interestingly, one researcher has previously suggested using intermittent fasting along with supplementary medium-chain triglycerides as a possible method to prevent or reduce the severity of SARS-CoV-2 infection.
Often the expected benefits are increased mitochondrial resistance to stress, better antioxidant activity, greater DNA repair and autophagy of damaged cells, and insulin sensitivity. These chime in with the health benefits of keto diets.
Ketogenic diets or KDs have been widely used to reduce body mass in severe obesity, metabolic disorders, migraine, and cancers, with adjustments in the composition of the overall pattern. In one particular group of very obese individuals who are at risk of cardiovascular disease, a very-low-calorie ketogenic diet (VLCKD) has been found to be very useful, supplying adequate nutrition while restricting carbohydrates to 30 g/day, making up the energy deficit by fat and protein. The daily caloric intake is reduced to 800kcal/day or less.
Interestingly, these individuals have been shown to regain insulin sensitivity, good glycemic control and normal blood pressure, as they lose primarily fat mass, preserving muscle mass.
Ketogenic diets also treats metabolic (dysfunction) associated fatty liver disease (MAFLD), with a healthy reduction in the liver fat content and insulin resistance in the liver within a week of treatment. Short VLCKD regimens also improve glycemic control in type 2 diabetes mellitus, since the very low carbohydrate intake not only promotes weight loss, and prevents blood sugar spikes, but promotes hepatic insulin sensitivity, thus preventing the synthesis of glucose in the liver. These changes cause a marked improvement in beta-cell function. The extremely rapid pace of change requires such diets be followed under strict medical supervision.
Ketogenic diets also increase ketone body levels in plasma, including acetoacetate and betahydroxybutyrate. These can provide fuel for energy as well as upregulating genes that control oxidative stress. They also prevent muscle cell breakdown and reduce inflammation, in addition to immunomodulatory effects, thus exhibiting a broad spectrum of action in different tissues.
Significantly ketone bodies inhibit inflammasome activation in response to viral infections, and could thus prevent the hyperinflammatory reaction associated with the cytokine storm in severe and critical COVID-19. Interestingly, M1 macrophages are known to be dependent on a supply of glucose for aerobic glycolysis. KDs could prevent their activation by drastically reducing the carbohydrate supply, while simultaneously sustaining M2 anti-inflammatory macrophages that use free fatty acids instead.
Ketogenic diets also promotes expansion of a specific type of T cell bearing γδ receptors. These γδ T cell receptor-bearing cells have immunomodulatory and anti-inflammatory activity. Perhaps they may be important in sustaining the lung epithelial barrier against this infection in the lung and in fat tissue. But only endogenous ketone bodies were able to protect mice against influenza, indicating the potential of KD to increase ketone bodies in a physiological manner and thus enhance the capacity of adaptive immune cells to prevent SARS-CoV-2 infection.
Very-low-calorie ketogenic diets or VLCKD also helps lower blood pressure via increased sodium losses through urine in combination with ketonuria. Physical exercise would further increase the favorable effects of such a diet. Attention should be paid to setting up properly customized KDs to produce a permanent lifestyle modification in obese patients, reducing multiple risk factors for severe COVID-19 through multiple mechanisms.
The authors concluded, “We believe that KD-induced increase in endogenous ketone bodies could represent a more valuable strategy to prevent Sars-Cov2 infection and adverse outcomes in obese patients, particularly in the current context of a prolonged pandemic emergency. Indeed, prevention and/or correction of all risk conditions associated with serious COVID-19 disease (obesity, hyperglycemia, high glycemic variability, insulin resistance, hypertension) is mandatory, in consideration of new waves of infections, in the absence of effective pharmacological therapies and vaccination. This could be obtained with a nutritional strategy aimed to induce fat mass loss, to reduce chronic inflammation, hepatic and systemic insulin resistance, and to improve nutritional status, cardiovascular health, immune response, glucose homeostasis and blood pressure control. Finally, the adoption of a well-structured and personalized KD regimen could help a progressive nutritional education and rehabilitation in obese patients, providing an effective tool to modify lifestyle behavior, supporting a long-term control of body weight, and favoring a reduction in all associated risk factors for potentially severe complications related to Sars-Cov2 infection. Well-designed multicentric studies on the actual incidence of severe COVID-19 disease among obese patients who followed or not a structured protocol of KD, could be helpful to confirm such hypothesis.”
For more on
Diets And Nutrition, keep on logging to Thailand Medical News.