Doctors Warn That Mild COVID-19 Can Cause Retroperitoneal Hemorrhage Due to Median Arcuate Ligament Syndrome
Nikhil Prasad Fact checked by:Thailand Medical News Team Nov 22, 2024 4 months, 3 weeks, 4 days, 19 hours, 16 minutes ago
Medical News: A New and Alarming Health Concern
Doctors in Japan have brought attention to a concerning medical phenomenon where COVID-19 might trigger a rare but serious condition: retroperitoneal hemorrhage associated with Median Arcuate Ligament Syndrome (MALS). The findings come from a case series conducted by researchers from Kansai Medical University Medical Center and Kansai Medical University Hospital in Osaka, Japan.
I
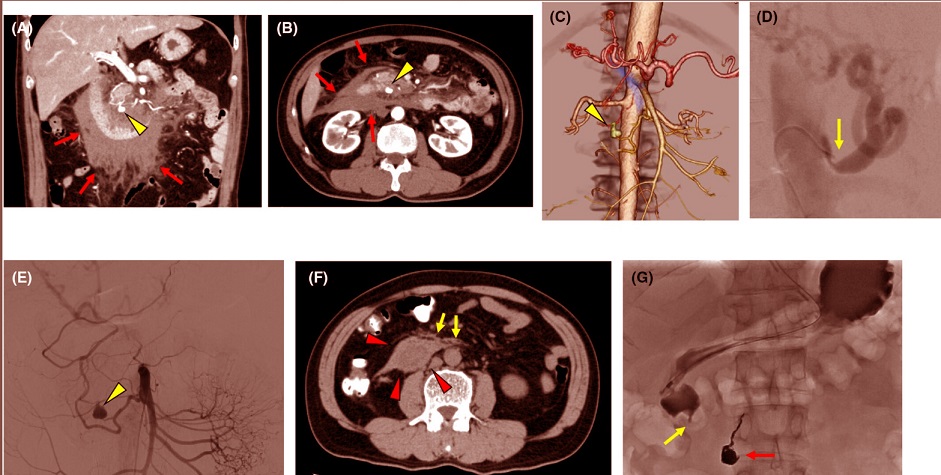
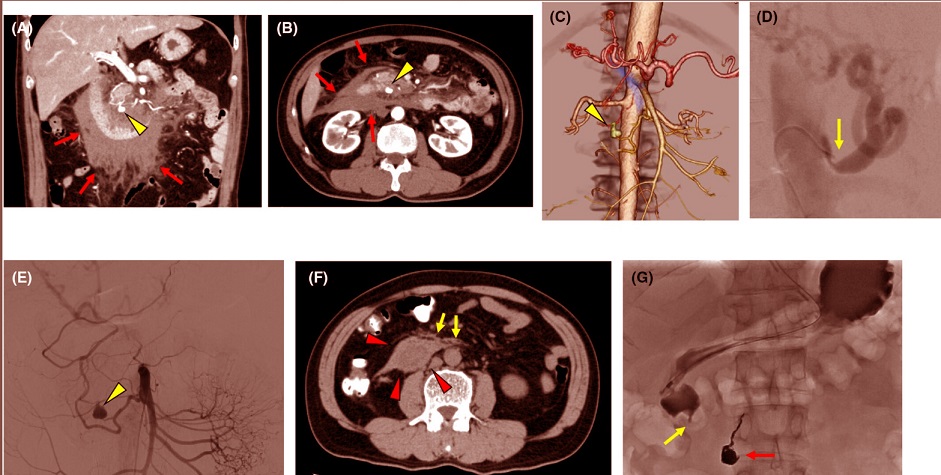
mages of retroperitoneal hemorrhage induced by visceral aneurysm rupture formed by median arcuate ligament syndrome in case 5. (A–C) Axial, coronal, and 3D computed tomography (CT) images on Day 2 of sickness show evidence of retroperitoneal hemorrhage (red arrows) with pseudoaneurysm of the inferior pancreaticoduodenal artery (yellow arrowhead). (D) Celiac artery angiographic image on Day 3 of sickness reveals the almost occluded celiac arterial root and post-stenotic dilation (yellow arrow). (E) Superior mesenteric artery angiography on the Day 3 image reveals a pseudoaneurysm of the inferior pancreaticoduodenal artery (yellow arrowhead). (F) Axial CT image on Day 13 reveals retroperitoneal hematoma (red arrowheads) and duodenal compression (yellow arrows). (G) Upper gastrointestinal series image on Day 13 reveals disruption in the duodenum (yellow arrow) and the coil placed for the pseudoaneurysm of the inferior pancreaticoduodenal artery (red arrow).
MALS is a rare disorder caused by the compression of the celiac artery by the median arcuate ligament. This compression leads to restricted blood flow, which forces nearby arteries to compensate, potentially causing aneurysms in the surrounding blood vessels. When these aneurysms rupture, they can result in life-threatening retroperitoneal hemorrhages.
COVID-19’s Role in Triggering Retroperitoneal Hemorrhage
In their study, Japanese doctors identified six cases of retroperitoneal hemorrhage in COVID-19 patients, marking what they believe to be the first documentation of this occurrence globally. To provide context, the Kansai Medical University Medical Center treated 1,490 COVID-19 patients between January 2020 and September 2022. Among these, six patients (0.4%) developed retroperitoneal hemorrhage linked to MALS, highlighting a rare but potentially severe complication.
The six patients, aged 41 to 74, included four men and two women. None had previously been diagnosed with MALS, and the hemorrhages occurred within three to nine days of COVID-19 symptom onset. Notably, all patients had mild cases of COVID-19, with only one showing pneumonia symptoms. Advanced imaging techniques, such as contrast-enhanced computed tomography (CE-CT), confirmed the presence of retroperitoneal hemorrhages and aneurysms linked to MALS.
This
Medical News report delves into the detailed findings of these cases, offering new insights into the interaction between COVID-19 and vascular health. The connection between COVID-19 and MALS-related complications appears to stem from the virus’s effects on vascular tissues. SARS-CoV-2, the virus responsible for COVID-19, is known to infect endothelial cells, le
ading to inflammation and increased levels of angiotensin II, a compound linked to aneurysm formation.
Treatment Strategies and Outcomes
Treatment in these cases primarily involved transcatheter arterial embolization (TAE), a minimally invasive procedure that stops bleeding by blocking blood flow to the ruptured vessel. Five of the six patients underwent TAE, with four receiving embolization using coils and one treated with an antibiotic-based embolic agent. The sixth patient underwent monitoring, as their aneurysm resolved without intervention.
Elective surgeries to remove the median arcuate ligament were performed in two patients to address the underlying issue. The other patients were managed conservatively, with regular follow-ups showing no recurrence of bleeding.
Complications were rare but significant: one patient developed duodenal stenosis due to hematoma compression, and another experienced portal vein thrombosis.
A Closer Look at a Typical Case
One of the more illustrative cases involved a 56-year-old man with no pre-existing medical conditions. He was diagnosed with COVID-19 and, two days later, experienced severe abdominal pain. Imaging revealed a ruptured pseudoaneurysm in the inferior pancreaticoduodenal artery caused by MALS. The rupture was treated successfully with coil embolization, and the patient recovered fully within weeks. However, he returned to the hospital with vomiting caused by duodenal compression from a shrinking hematoma. This issue resolved with non-surgical interventions, and the patient remained healthy during follow-ups for over 20 months.
Broader Implications and Future Directions
While retroperitoneal hemorrhage is a rare complication, its association with COVID-19 underscores the need for heightened awareness among healthcare providers. The study authors noted that the condition occurred most frequently during waves of COVID-19 dominated by the Delta and Omicron variants. Although the number of cases was small, the findings suggest a possible link between specific viral strains and vascular complications.
Importantly, the study raises questions about the necessity of surgical interventions like median arcuate ligament resection. While some experts advocate for the procedure to prevent future aneurysm formation, the Japanese team found that careful monitoring and non-surgical management could yield favorable outcomes in selected cases. However, the researchers emphasized that their conclusions are based on limited follow-up periods, and longer-term studies are needed.
Key Takeaways for Patients and Clinicians
The study offers several takeaways for both medical professionals and the general public:
-Awareness of Symptoms: For patients with COVID-19 presenting with unexplained abdominal pain, healthcare providers should consider imaging studies to rule out MALS-related hemorrhage.
-Importance of Early Diagnosis: Early identification of retroperitoneal hemorrhage is critical for effective treatment and preventing severe complications.
-Long-Term Monitoring: Patients diagnosed with MALS or treated for retroperitoneal hemorrhage require regular follow-ups to monitor for potential recurrences or complications.
Conclusion
This case series serves as an important reminder of the far-reaching effects of COVID-19 on human health. While the virus is primarily known for its respiratory complications, its impact on vascular systems is becoming increasingly evident. The study highlights a rare but significant complication that underscores the need for multidisciplinary care in managing COVID-19 patients. By drawing attention to these findings, the researchers aim to improve patient outcomes and inform future treatment protocols.
The study findings were published in the peer-reviewed journal: Acute Medicine & Surgery.
https://onlinelibrary.wiley.com/doi/10.1002/ams2.70015
For the latest COVID-19 News, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/covid-19-can-cause-cervical-arterial-dissections-or-tears-in-the-wall-of-the-large-blood-vessel-in-the-neck
https://www.thailandmedical.news/news/doctors-warn-that-covid-19-can-cause-spontaneous-esophageal-rupture
https://www.thailandmedical.news/news/covid-19-causes-coronary-artery-lesions-and-plaque-ruptures-in-coronary-artery-disease-patients
https://www.thailandmedical.news/news/doctors-warn-that-covid-19-infections-can-cause-spontaneous-tears-dissections-in-the-walls-of-the-coronary-artery
https://www.thailandmedical.news/news/covid-19-news-researchers-warn-that-sars-cov-2-infections-can-lead-to-splenic-infarctions
https://www.thailandmedical.news/news/warning-sars-cov-2-infections-causes-intestinal-ischemia-increases-disease-severity-and-risk-of-mortality
https://www.thailandmedical.news/news/breaking-pediatricians-warn-that-covid-19-can-cause-gastric-perforations-in-new-borns
https://www.thailandmedical.news/news/breaking-covid-19-news-case-study-shows-that-even-asymptomatic-sars-cov-2-infections-can-lead-to-spontaneous-bowel-perforations