For The Latest Medical News, Health News, Research News, COVID-19 News, Pharma News, Glaucoma News, Diabetes News, Herb News, Phytochemical News, Thailand Cannabis News, Cancer News, Doctor News, Thailand Hospital News, Oral Cancer News, Thailand Doctors

A number of things can increase your risk of dry eyes. These include:
When working at a computer or using a smartphone or other portable digital device, we tend to blink our eyes less fully and less frequently, which leads to greater tear evaporation and increased risk of dry eye symptoms.
Dry eye syndrome can occur at any age, but it becomes increasingly more common later in life, especially after age 50.
Post-menopausal women are at greater risk of dry eyes than men of the same age.
Though it can be difficult to determine the exact extent that contact lens wear contributes to dry eye problems, dry eye discomfort is a primary reason why people discontinue contact lens wear.
Air conditioning, ceiling fans and forced air heating systems all can decrease indoor humidity and/or hasten tear evaporation, causing dry eye symptoms.
Arid climates and dry or windy conditions increase dry eye risks.
The air in the cabins of airplanes is extremely dry and can lead to dry eye problems, especially among frequent flyers.
In addition to dry eyes, smoking has been linked to serious eye problems, including macular degeneration, cataracts and uveitis. Smoke from incense sticks or joss sticks are just as bad.
Certain systemic diseases such as diabetes, thyroid-associated diseases, lupus, rheumatoid arthritis and Sjogren's syndrome,contribute to dry eye problems.
Many prescription and nonprescription medicines including antihistamines, antidepressants, certain blood pressure medications and birth control pills increase the risk of dry eye symptoms.
Incomplete closure of the eyelids when blinking or sleeping — a condition called lagophthalmos, which can be caused by aging or occur after cosmetic blepharoplasty or other causes, can cause severe dry eyes that can lead to a corneal ulcer if left untreated.
LASIK and other corneal refractive surgery can sometimes cause dry eyes. In most cases, however, dry eye discomfort after LASIK is temporary and resolves within a few weeks of the procedure. If you have dry eyes prior to LASIK, your eye doctor may recommend a dry eye treatment regimen before your procedure to insure the best possible LASIK results.
Researchers in Korea evaluated risk factors for dry eye disease among schoolchildren who used video devices, including smartphones and discovered that children using smartphones could them to develop dry eye disease at an early age. The study authors concluded that smartphone use in children was strongly associated with pediatric dry eye disease. Older-grade students in urban environments had the greatest risk factors and prevalence of DED. The authors also pointed out that signs and symptoms of dry eyes improved when smartphone use was discontinued, and that increased outdoor activities appeared to be protective against pediatric dry eye disease.
The only manner to know for sure if you've got chronic dry eye syndrome is to have your eye doctor perform one or more dry eye tests during an eye exam.
Symptoms alone are poor predictors of the presence and severity of dry eye disease. Symptoms can vary significantly from person to person, and may even be affected by personality type. Some people with only minimal or mild dry eyes may feel their eyes are very bothersome, while others may have significant dry eye problems and not consider their symptoms significant enough to see an eye doctor.
Only a careful examination of your eyes by an eye doctor can reveal the presence and severity of dry eye syndrome and help your doctor determine the best type of dry eye treatment to keep your eyes healthy, comfortable and seeing well. Tests and procedures that may be used to determine the cause of your dry eyes include:
An eye exam that includes a complete history of your overall health and your eye health can help your doctor diagnose the cause of your dry eyes.
Your doctor may measure your tear production using the Schirmer test. In this test, blotting strips of paper are placed under your lower eyelids. After five minutes your doctor measures the amount of strip soaked by your tears.
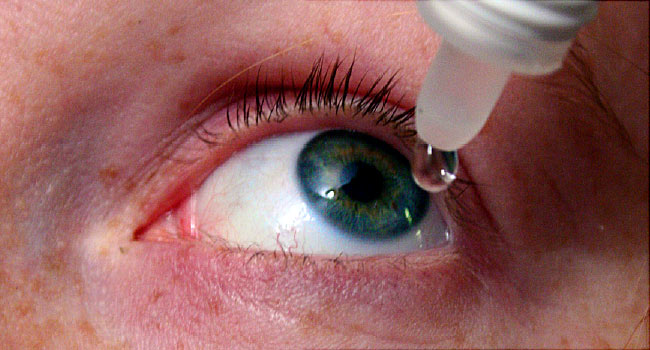
Other tests use special dyes in eyedrops to determine the surface condition of your eyes. Your doctor looks for staining patterns on the corneas and measures how long it takes before your tears evaporate.
Thankfully, there are effective treatment options if you suffer from chronic dry eye
In many cases, routine use of artificial tears and minor behavioral modifications (taking frequent breaks during computer use, for example) can significantly reduce dry eye symptoms. In other cases, your eye doctor might recommend prescription eye medications and in-office procedures to help your body create and secrete more tears and to decrease eye irritation and inflammation.
The following below is a list of dry eye treatments that are commonly used by eye doctors to reduce the signs and symptoms of dry eyes. Your eye doctor may recommend only one of these dry eye treatments or a combination of treatments, depending on the cause(s) and severity of your condition.
For mild cases of dry eye caused by computer use, reading, schoolwork and other situational causes, the best dry eye treatment may simply be frequent use of artificial tears or other lubricating eye drops.
There are many brands of artificial tears that are available without a prescription. The challenge with using artificial tears is not lack of product availability but it's the confusing number of brands and formulations available to choose from.
Artificial tears and other over-the-counter (OTC) lubricating eye drops are available in a wide variety of ingredients and viscosity ("thickness").
Artificial tears with low viscosity are "thin" and watery. They often provide quick relief with little or no blurring of your vision when you apply them. But often their soothing effect is very short-lived, and sometimes you must use these drops very frequently to get adequate dry eye relief.
On the other hand, artificial tears that have a high viscosity are more gel-like and can provide longer-lasting lubrication. But typically these drops cause significant blurring of your vision for several minutes immediately after you apply them. For this reason, these drops often are not a good choice for use during your work day or when you need immediate clear vision for tasks such as driving. Sometimes high-viscosity artificial tears are recommended for bedtime use only.
Also, the ingredients in certain brands of artificial tears may determine which type of dry eye condition they are better suited for. For example, one brand might work better if you don't produce enough natural tears (aqueous-deficiency dry eye) while another brand may be more effective if your natural tears evaporate too quickly (evaporative dry eye).
If your eye doctor recommends that you use one or more brands or formulations of artificial tears, be sure to follow the directions he or she gives you concerning when and how often you use them. Also, do not substitute other brands from those your eye doctor recommends. Using a different brand or multiple brands of artificial tears will make it difficult to assess the success of the dry eye treatment your doctor recommended.
Instead of OTC artificial tears (or in addition to them), your eye doctor might recommend daily use of a prescription eye drop called Restasis (Allergan) for your dry eye treatment.
Restasis does more than simply lubricate the surface of your eye. It includes an agent that reduces inflammation associated with dry eye syndrome and helps your body produce more natural tears to keep your eyes moist, comfortable and healthy.
It's important to know, however, that the therapeutic effect of Restasis is not immediate. You must use the drops daily for a minimum of 90 days to experience the full benefits of this dry eye treatment.
Some people who try Restasis will experience burning eyes early during the first few weeks of treatment.
Xiidra is another prescription eye drop for dry eye treatment. Xiidra like Restasis, is aimed at reducing inflammation associated with the signs and symptoms of dry eyes.
The safety and efficacy of Xiidra was studied in four placebo-controlled, 12-week clinical trials that included 1,181 people with dry eyes. Participants were evaluated for dry eye signs and symptoms just prior to starting use of the drops, then after two weeks, six weeks and 12 weeks of Xiidra use.
In two of the four studies, participants noticed a significant reduction in dry eye symptoms after using Xiidra for two weeks. In all four studies, participants noticed a larger reduction in dryness symptoms after six weeks and 12 weeks of Xiidra use.
Also, at 12 weeks, a statistically significant reduction in signs of dry eyes was found among Xiidra users compared with participants given a placebo in two of the four studies.
The most common side effects of Xiidra reported in the studies were eye irritation, altered taste sensation and reduced visual acuity, which occurred in 5% to 25% of participants.
The recommended dosage for Xiidra, like Restasis, is two applications in each eye per day, approximately 12 hours apart.
Over the past several years, inflammation has been recognized as a significant cause of dry eyes. Inflammation frequently causes the redness and burning associated with dry eye disease.
Artificial tears usually do not adequately address these inflammatory changes, and your doctor may recommend steroid eye drops to better manage the underlying inflammation associated with dry eyes.
Steroid eye drops generally are used short-term to quickly manage symptoms. They often are used in conjunction with artificial tears and Restasis or Xiidra, as a complement to these more long-term dry eye treatment strategies.
Steroid eye drops (especially if used for relatively long periods) have the potential of causing side effects. So, it's important to make your eye doctor aware of your full medical history before starting steroid eye drops.
For example, steroid eye drops can increase the risk of developing high eye pressure or even cataracts if used for extended periods of time. But these risks are low when the drops are used only on a short-term basis for dry eye treatment.E
Extended usage of steroids have also been credited with increasing the incidence ocular herpes for those already carrying the virus.
Lacrisert (Bausch + Lomb) is a sterile, slow-release lubricant that is placed under the lower eye lid where the conjunctiva of the inside of the eyelid meets the conjunctiva of the eyeball.
It is a solid insert composed of a preservative-free lubricating agent (hydroxypropyl cellulose) that slowly liquefies over time, providing an all-day moistening effect.
For most people with dry eyes, a single Lacrisert is applied once a day. The device has been proven to relieve dryness, burning, watery eyes, foreign body sensation, itching, light sensitivity and blurred vision, according to the company. Lacrisert typically is recommended for patients with moderate to severe dry eye symptoms, especially if dry eye treatment with artificial tears alone proves unsuccessful.
Should the Lacrisert be placed under the eyelid improperly, it's possible Lacrisert can cause a corneal abrasion. Also, Lacrisert may cause transient blurred vision, eye discomfort or irritation, matting or stickiness of eyelashes, red eyes and sensitivity to light.
Punctal plugs sometimes are used in dry eye treatment to help tears remain on the surface of the eye longer. A punctal plug is a small, sterile device that is inserted into one of the small openings
(puncta) of tear drainage ducts that are located in the inner corner of the upper and lower eyelids.
After these openings have been plugged, tears can no longer drain away from the eye through these ducts. This results in the tear film remaining intact longer on the surface of the eye, relieving dry eye symptoms.
So where do the tears go? Usually they will simply evaporate from the eye surface without symptoms. But if insertion of punctal plugs causes watery eyes, one or more of the plugs can be removed.
A very significant percentage of dry eye cases are caused by inadequate oil (meibum) being secreted from meibomian glands located along the margin of the eyelids.
The openings of these glands are near the base of the eyelashes. If these openings get clogged, the oil that's critical to keeping the tear film from evaporating too quickly cannot do its job. This is called meibomian gland dysfunction (MGD), which is a significant cause of evaporative dry eye symptoms.
To treat MGD and evaporative dry eye, your eye physician may perform an in-office procedure called meibomian gland expression. In this procedure, warm compresses may or may not first be applied to your eyelids; then a forceps-type device is used to squeeze the clogged contents (hardened meibum and possibly other substances) from the meibomian glands.
To fully express the contents of the meibomian glands and get them functioning properly, significant pressure must be applied to the eyelids, which can be uncomfortable. But the results usually make any short-term discomfort from the procedure worth it.
A better alternative (and potentially more comfortable) way to help open clogged meibomian glands to treat dry eyes is to simply apply warm compresses to the closed eyelids to soften the hardened meibum.
Unfortunately, for warm compresses to work well, some researchers say you have to use a compress that can maintain a temperature of 108 degrees Fahrenheit for more than 10 minutes, and the compresses have to be applied for this length of time at least twice a day.
Most people are unable or unwilling to perform this type of dry eye treatment correctly, and shorter and less frequent use of variable-temperature warm compresses typically is ineffective.
The LipiFlow Thermal Pulsation System (TearScience) is an automated, in-office dry eye treatment that combines the best features of warm compress therapy and meibomian gland expression.
The patented device fits over the eyelids and applies precisely-controlled heat to the lids to soften hardened meibum trapped in the meibomian glands. At the same time, the LipiFlow system applies pulsed pressure to the eyelids to open and express the clogged glands, thereby restoring the correct balance of oils in the tear film to relieve dry eye syndrome.
Lipiflow treatment takes approximately 12 minutes per eye. In a clinical study of the effectiveness of the procedure, 76% of patients reported improvement of their dry eye symptoms within two weeks of treatment. Most patients also showed improvement in the quality and quantity of meibomian gland secretions and the duration of time their tear film remained on the eye before evaporating. In some cases, however, it can take a few months for improvements from the LipiFlow procedure to become apparent. Typically, the beneficial effects of the LipiFlow procedure last one to three years or longer.
Potential side effects from LipiFlow dry eye treatment include corneal abrasion, eye pain, swollen eyelids, eyelid irritation or inflammation, chalazion, transient blurred vision, itching, and red eyes.
The US FDA has approved the use of intense pulsed light (IPL) to treat rosacea on the skin. Rosacea on the skin and eyelid often occur together. Ocular rosacea is characterized by dilated blood vessels coursing along the eyelash margin in patients suffering from blepharitis and may contribute to dry eye symptoms.
In IPL treatment, a hand-held device flashes bright light onto the skin. The light is filtered to allow only wavelengths that can be absorbed by the dilated blood vessels. The effect of this treatment may be the resolution of the dilated vessels and associated inflammation that contributes to dry eye symptoms.
Many patients experience relief from their dry eye symptoms after IPL and become less dependent on artificial tears and other routine measures to keep their eyes comfortable. For this reason, IPL treatment may be well-suited for dry eye patients who don't want to be troubled by the inconvenience of frequent eye drop use.
Patients usually require four to six monthly IPL treatments for optimum effects. Typically, the treatments are well-tolerated and are not associated with any down-time. However, it's important to discuss with your doctor how much time you spend in the sun, as the treatments will make your eyelids more light-sensitive.
It may not be appropriate for patients with certain skin pigmentations.
Doctors sometimes recommend nutritional supplements as part of a holistic dry eye treatment plan. Studies have found that supplements containing omega-3 fatty acids can decrease dry eye symptoms. Good sources of omega-3s include cold-water fish such as salmon, sardines, herring and cod. For a vegetarian source of omega-3s, some eye doctors recommend flaxseed oil to relieve dry eye. We at Thailand Medical News can vouch that we found this useful as about 7 of our staff who had dry eyes syndrome got relieve by taking a high dose Omega 3 Fish oil and also the symptoms disappeared after a while. But please consult a physician prior to taking any medications or supplements as Omega 3 can act as a blood thinner for some.
Also, simply drinking more water might help relieve dry eye symptoms. Mild dehydration often
makes dry eye problems worse. This is especially true during hot, dry and windy weather.
If you have mild dry eye symptoms, there are several things you can try to get relief before going to the eye doctor:
Research has shown that people tend to blink much less frequently than normal when viewing a computer, smartphone or other digital display. This decreased blink rate can cause or worsen dry eye symptoms. Make a conscious effort to blink more often when using these devices. Also, perform full blinks, gently squeezing your eyelids together to fully spread a fresh layer of tears over your eyes.
style eyewear with side shields can protect your eyes from moisture-robbing wind and irritating debris.
A good rule of thumb here is to look away from your screen at least every 20 minutes and look at something that is at least 20 feet from your eyes for at least 20 seconds. Eye doctors call this the "20-20-20 rule," and abiding by it can help relieve dry eyes and computer eye strain.
Eyeliner and other eye makeup can clog the openings of the meibomian glands at the base of the eyelashes, leading to meibomian gland dysfunction and evaporative dry eye. At the end of the day, be diligent about remove all traces of makeup from your lids and lashes.
When washing your face before bedtime, gently wash your eyelids to remove bacteria that can cause blepharitis and meibomian gland problems that lead to dry eye symptoms. Apply a warm, moist washcloth to your closed lids for at least 20 seconds. Then gently wash your lids and lashes with a mild cleanser, such as diluted baby shampoo or pre-moistened eyelid wipes sold in drugstores.
When outdoors in daylight hours, always wear sunglasses that block 100% of the sun's UV rays. For the best protection, choose sunglasses that also feature a wrap-style frame to protect your eyes from wind, dust and other irritants that can cause or worsen dry eye symptoms.
In addition to the dry eye treatments listed above, your eye doctor may recommend one or more of the following supplemental measures if any of the conditions below apply to you:
Many medicines including antihistamines, antidepressants, birth control pills, certain blood pressure medications and more can cause or worsen dry eye symptoms. Even over-the-counter (nonprescription) medications for allergies and other conditions can cause dry eyes.
Make sure to discuss all medications you are taking with your eye doctor or ophthalmologists if you are experiencing dry eye problems. In some cases, adjusting the type and number of medications you are taking may help reduce dry eye symptoms without causing adverse health effects.
Never discontinue a prescription medication without first discussing the matter with your doctor. If your eye doctor feels an adjustment to one of your medications may help relieve dry eye symptoms, he or she can discuss it with your physician to see if such a change is possible.
Treating eyelid conditions. If you have blepharitis, meibomian gland dysfunction or other eyelid conditions, these often are associated with dry eye disease and should be addressed as part of your overall dry eye treatment regimen. For example, if you have blepharitis, your eye doctor may recommend use of an antibiotic and/or steroid ointment or eye drop in addition to daily eyelid cleansing with a non-irritating shampoo.
Discontinuing or reducing contact lens wear. If you wear contact lenses, it can be difficult to tell if an underlying dry eye condition is causing contact lens discomfort or if your contact lenses are causing dry eye symptoms. If you wear contacts, it's often best to discontinue wearing them (or perhaps switch to daily disposable contact lenses) while your dry eye treatment is in progress.
Here’s a look at a few complications that can occur if you are not properly treating chronic dry eye diseases or fail to consult a doctor.
A corneal ulcer is an open sore that develops on your cornea, which is the clear, protective outer layer of your eyes. These ulcers typically occur after an injury, but severely dry eyes can also play a role.
Debris like dirt and other particles can sometimes get into your eyes. If your tear glands don’t produce enough tears, your eyes might be unable to wash the particles away.
Debris can then scratch the surface of your cornea. If bacteria gets into the scratch, an infection can develop, causing an ulcer.
Corneal ulcers are treatable with antibiotic eye drops. But if left untreated, these ulcers can spread and scar the eyeball, causing partial or complete blindness.
Untreated dry eye can also lead to inflammation of the conjunctiva. This is the clear layer of cells that cover the white part of your eyeball and the inner surface of your eyelids. This type of inflammation is known as conjunctivitis.
Symptoms include redness, light sensitivity, and a gritty feeling in the eyes. This type of conjunctivitis is different from bacterial conjunctivitis. It’s usually milder and doesn’t require treatment, although you should see an eye doctor for inflammation that does not improve or worsens.
For contact lenses to feel comfortable, your eyes need to produce enough tears. If not, your contact lenses can become overly dry. This can lead to irritation, a gritty sensation, and redness.
Dry contact lenses can also stick to your eyeball, making it difficult to remove them. Because contacts need moisture, chronic dry eye may prevent you from wearing your lenses. You may have to wear eyeglasses instead.
If your vision becomes blurry, you may think your eyes have changed and you need a stronger prescription for your eyeglasses or contacts.
But sometimes, blurry vision is a symptom of chronic dry eye. If left untreated, blurriness may gradually worsen, or you could develop double vision.
If so, you may have trouble driving a car and reading. Sometimes, even working can become difficult or impossible with blurry vision.
Depending on the severity of dry eye, you may have difficulty keeping your eyes open. This can happen if you have the sensation that something is in your eye or if you have extreme light sensitivity.
Artificial tears may provide some moisture to help open your eyes, but you might be unable to fully open them. You may squint, especially when exposed to sunlight or computer light. An inability to keep your eyes open als makes driving imposssible.
More research is needed, but there appears to be a connection between dry eyes and headaches. Even though the relationship isn’t fully understood, some people diagnosed with dry eye also experience headaches.
One recent study found that people who live with migraine headaches are more likely to have dry eyes compared to the general population.
Dealing with chronic headaches can affect every area of your life. It may become difficult to concentrate and enjoy your favorite activities with your family and friends. It can also affect your productivity at work and school.
There’s also a connection between untreated dry eye and depression. Because dry eye syndrome can affect your quality of life, making it difficult to perform everyday activities, it can affect your emotional well-being.
One recent study evaluated the relationship between dry eye disease and depressive symptoms in over 6,000 women. Researchers found that women diagnosed with dry eye had a higher likelihood of developing psychological stress, depressive moods, and anxiety.
The connection isn’t fully understood. It could be that some medications for treating depression having a drying effect on the eyes, or that dry eyes limit activity to the point where a person becomes withdrawn, anxious, and depressed.
If the latter is true, it appears that chronic dry eye can affect emotional health in the same way that other chronic conditions affect mood.
Chronic dry eye is a common problem, but it can lead to severe complications if left untreated. Some individuals are able to resolve dry eyes with over-the-counter artificial tears. Always consult a doctor or ophthalmologist . The right therapy can increase the quality of your tears and improve the quality of your life. Neglected or mistreated conditions can even lead to blindness.