Dysfunctional Insulin Receptor Signaling System Found to Play Key Role in Chronic Pain and Diabetes in Long COVID Patients
Nikhil Prasad Fact checked by:Thailand Medical News Team Dec 03, 2024 1 year, 4 days, 5 hours, 52 minutes ago
Medical News: A new study by researchers from Foshan University, China, and the Cancer Hospital of the Chinese Academy of Medical Sciences, Beijing, delves into the intricate relationship between long COVID, diabetes, and chronic pain. The study emphasizes the role of the dysfunctional insulin receptor signaling system (IRSS) in exacerbating these conditions. Patients with diabetes and chronic pain often experience heightened health challenges after recovering from COVID-19, making this research a critical piece in understanding the post-viral syndrome.
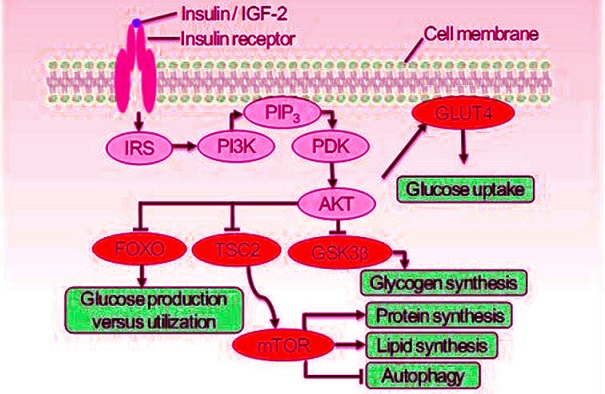
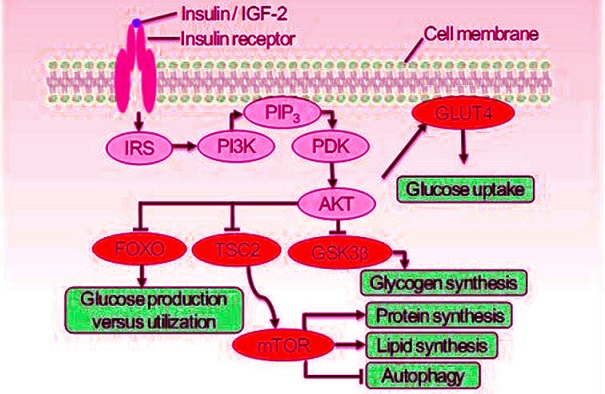 The insulin receptor signaling system (IRSS) and partial of its physiological function. Once the insulin receptor (IR) tyrosine kinase is activated by insulin or IGF-2, it causes tyrosine phosphorylation of IR and of the IR substrate (IRS) proteins. Phosphotyrosine sites on IRS allow binding of the lipid kinase PI3K, which synthesizes PtdIns(3,4,5)P3 (PIP3) at the cytomembrane. This recruits the phosphoinositide-dependent kinase (PDK), which directly phosphorylates the Thr308 residue of AKT. Activated AKT goes on to translocate GLUT4 to cytomembrane thus let glucose entering the cell, and inhibit the glycogen synthase kinase 3β (GSK3β), the forkhead family box O (FOXO) transcription factors, and the protein tuberous sclerosis 2 (TSC2) which permits activation of mTOR. These effector proteins mediate the effects of insulin on glucose production, utilization and uptake, the synthesis of glycogen, protein and lipid, as well as the cellular autophagy.
The insulin receptor signaling system (IRSS) and partial of its physiological function. Once the insulin receptor (IR) tyrosine kinase is activated by insulin or IGF-2, it causes tyrosine phosphorylation of IR and of the IR substrate (IRS) proteins. Phosphotyrosine sites on IRS allow binding of the lipid kinase PI3K, which synthesizes PtdIns(3,4,5)P3 (PIP3) at the cytomembrane. This recruits the phosphoinositide-dependent kinase (PDK), which directly phosphorylates the Thr308 residue of AKT. Activated AKT goes on to translocate GLUT4 to cytomembrane thus let glucose entering the cell, and inhibit the glycogen synthase kinase 3β (GSK3β), the forkhead family box O (FOXO) transcription factors, and the protein tuberous sclerosis 2 (TSC2) which permits activation of mTOR. These effector proteins mediate the effects of insulin on glucose production, utilization and uptake, the synthesis of glycogen, protein and lipid, as well as the cellular autophagy.
This
Medical News report sheds light on how the SARS-CoV-2 virus worsens metabolic and neural conditions. Researchers point to the insulin receptor as a key player, detailing its involvement in metabolic regulation and the pathogenesis of chronic pain, especially in patients with Type 2 Diabetes Mellitus (T2D).
Understanding the Insulin Receptor and Its Dysfunction in COVID-19
The insulin receptor, a crucial component of the body's metabolic machinery, facilitates glucose metabolism and regulates various cellular processes. However, SARS-CoV-2 directly affects this system by binding to ACE2 receptors, which are highly expressed in pancreatic beta cells. This interaction leads to reduced insulin secretion and impaired glucose metabolism.
Patients with T2D are particularly vulnerable, as pre-existing insulin resistance is compounded by the virus. Hypoxia, a common symptom of severe COVID-19, further worsens insulin receptor expression and function. This leads to a vicious cycle where impaired glucose metabolism feeds into the severity of chronic pain and systemic inflammation.
Chronic Pain and Its Connection to Metabolic Dysregulation
Long COVID is now recognized for its extensive sequelae, with chronic pain being one of the most commonly reported symptoms. Approximately 77% of long COVID patients experience some form of persistent pain. This includes musculoskeletal pain, neuropathy, and generalized discomfort, which significantly affects their quality of life.
The study highlights tha
t the dysfunction of the IRSS not only exacerbates chronic pain but also promotes the persistence of pain memory in the brain. This occurs through the disruption of neural circuits and synaptic plasticity, ultimately resulting in continuous pain sensations.
How Nerve Damage Influences Glucose Metabolism
The interaction between nerve injury and metabolic dysfunction is a critical area of focus in the study. The researchers found that nerve injuries, such as those caused by COVID-19, can lead to decreased insulin receptor expression in both central and peripheral tissues. This contributes to worsening glucose metabolism and accelerates the progression of diabetes.
In experimental models, rats with nerve injuries exhibited reduced insulin receptor activity and higher blood glucose levels. These findings align with clinical observations in COVID-19 patients who report severe neuralgia alongside worsening diabetes.
A Potential Solution in Transcutaneous Auricular Vagal Nerve Stimulation
One of the most promising findings of the study is the potential use of transcutaneous auricular vagal nerve stimulation (taVNS) to address these interconnected conditions. The technique involves non-invasive stimulation of the vagus nerve, which has shown significant benefits in both central and peripheral systems.
In clinical and preclinical studies, taVNS improved insulin receptor expression, alleviated chronic pain, and enhanced glucose metabolism. The researchers observed that taVNS induced rhythmic insulin secretion, which persisted for hours post-stimulation, optimizing glucose regulation and reducing inflammation.
Key Findings from the Study
-Bidirectional Impact of COVID-19 and Diabetes: The study confirms that SARS-CoV-2 exacerbates insulin resistance and glucose metabolism issues, creating a feedback loop with T2D.
-Central and Peripheral Dysfunctions: IRSS dysfunction affects both central neural circuits and peripheral tissues, aggravating chronic pain and metabolic issues.
-Impact of Nerve Injuries: COVID-19-induced nerve injuries further suppress insulin receptor activity, intensifying metabolic dysregulation.
-taVNS as a Therapeutic Option: The findings suggest that taVNS is not only safe but also effective in treating chronic pain and improving metabolic health in long COVID patients.
Conclusion
The study underlines the importance of addressing insulin receptor signaling dysfunction in managing long COVID symptoms, especially in patients with diabetes and chronic pain. By improving IRSS function, it may be possible to alleviate pain and metabolic disturbances in affected individuals.
Therapies like taVNS offer a non-invasive and promising approach to break the cycle of pain and metabolic dysregulation. The researchers emphasize the need for further clinical trials to establish the efficacy and safety of taVNS in broader patient populations.
Ultimately, this research highlights the interconnected nature of metabolic and neural health, showing how a single viral infection can have long-lasting impacts. For patients suffering from long COVID, such studies provide hope for more effective and targeted treatments in the future.
The study findings were published in the peer-reviewed journal: Frontiers in Pain Research.
https://www.frontiersin.org/journals/pain-research/articles/10.3389/fpain.2024.1486851/full
For the latest COVID-19 News, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/sars-cov-2-nucleocapsid-protein-found-to-worsen-chronic-pain-in-those-exposed-to-covid-19
https://www.thailandmedical.news/news/study-finds-that-42-6-percent-of-those-infected-with-covid-19-exhibit-persistent-musculoskeletal-pain
https://www.thailandmedical.news/news/cinnamon-extract-offers-hope-for-joint-pain-relief
https://www.thailandmedical.news/news/alpha-lipoic-acid-offers-new-hope-for-diabetic-pain-relief