Emerging Evidence Links COVID-19 to Rare Autoimmune Disorder Granulomatosis with Polyangiitis
Nikhil Prasad Fact checked by:Thailand Medical News Team Dec 20, 2024 3 months, 3 weeks, 5 days, 8 hours, 50 minutes ago
Medical News: The Complex Relationship Between COVID-19 and Autoimmunity
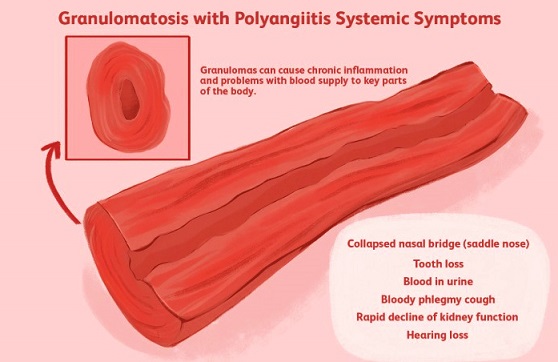
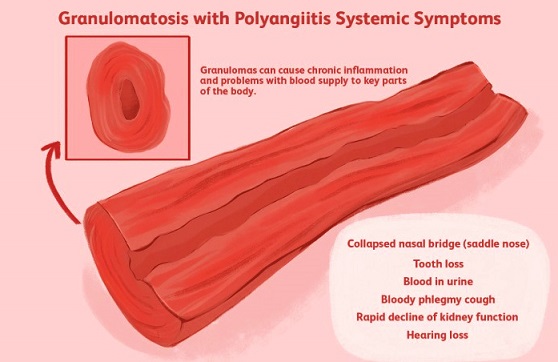
The COVID-19 pandemic has disrupted lives globally, with its effects extending beyond acute infection to potential long-term complications. One particularly concerning development is the emergence of autoimmune diseases in the aftermath of COVID-19. Among these conditions is granulomatosis with polyangiitis (GPA), a rare but severe autoimmune vasculitis.
 Emerging Evidence Links COVID-19 to Rare Autoimmune Disorder Granulomatosis with Polyangiitis
Emerging Evidence Links COVID-19 to Rare Autoimmune Disorder Granulomatosis with Polyangiitis
GPA, formerly known as Wegener’s disease, involves inflammation and necrosis of small to medium-sized blood vessels. It primarily affects the respiratory system and kidneys, leading to symptoms such as nasal congestion, sinusitis, coughing, and renal dysfunction. This
Medical News report explores how GPA is increasingly linked to COVID-19, with researchers identifying potential mechanisms behind this connection.
A recent case report highlights the onset of GPA in a 41-year-old man who had previously been hospitalized for severe COVID-19. Conducted at Zanjan University of Medical Sciences in Iran, this study offers insights into how SARS-CoV-2 infection may trigger or exacerbate autoimmune responses, contributing to the development of GPA. This article sheds light on these findings and their implications for medical practice and patient care.
A Rare Case of Post-COVID Autoimmune Disease
The case centers on a previously healthy middle-aged male who presented with fatigue, abdominal pain, shortness of breath, and gross hematuria. Notably, the patient had a history of severe COVID-19 infection requiring hospitalization one year prior. During his recent admission, he exhibited laboratory findings consistent with GPA, including elevated inflammatory markers (ESR and CRP), significant proteinuria, hematuria, and positive anti-neutrophil cytoplasmic antibodies (C-ANCA).
Clinical imaging further supported the diagnosis. High-resolution computed tomography (HRCT) of the lungs revealed bilateral ground-glass opacities, small nodules, and structural changes indicative of bronchiectasis. A kidney biopsy confirmed pauci-immune proliferative glomerulonephritis, a hallmark of GPA. Following immunosuppressive therapy with corticosteroids and cyclophosphamide, the patient’s symptoms improved, and he was discharged with a tapering regimen of medication and follow-up instructions.
Understanding the Mechanisms
The underlying mechanisms linking COVID-19 and GPA remain an active area of investigation. Researchers suggest that the immune dysregulation caused by SARS-CoV-2 may play a pivotal role. COVID-19 is known to trigger excessive production of pro-inflammatory cytokines, such as interleukins IL-1, IL-6, and IL-10, leading to a phenomenon commonly referred to as a cytokine storm. These inflammatory cascades can cause significant endothelial damage, exposing tissues to autoantibody attacks.
Additionally, molecular mimicry - where components of the virus resemble host proteins - may activate imm
une cells to target the body’s own tissues. The study also identified increased levels of neutrophil extracellular traps (NETs), which can damage blood vessels and contribute to the development of ANCA-associated vasculitis, including GPA. These findings suggest that COVID-19 may act as a catalyst for autoimmune diseases in genetically predisposed individuals.
Implications for Diagnosis and Treatment
The case underscores the importance of early diagnosis and treatment of GPA, particularly in post-COVID-19 patients presenting with unexplained respiratory or renal symptoms. Misdiagnosis can lead to delays in treatment, increasing the risk of severe complications such as diffuse alveolar hemorrhage, renal failure, and even death. Physicians should maintain a high index of suspicion for GPA in patients with persistent inflammatory symptoms and a history of COVID-19.
Immunosuppressive therapy, often involving systemic corticosteroids and cyclophosphamide, remains the cornerstone of GPA treatment. In severe cases with renal involvement, plasma exchange may be necessary. This case also highlights the critical role of multidisciplinary collaboration in managing GPA, given its complex and multisystemic nature.
Broader Context: Autoimmunity and COVID-19
Emerging evidence suggests that COVID-19 may not only trigger de novo autoimmune diseases but also exacerbate pre-existing conditions. For instance, several studies have documented cases of autoimmune phenomena following COVID-19 vaccination. While these instances are exceedingly rare and vaccines remain safe for the vast majority, they underscore the intricate relationship between immune activation and autoimmunity.
In this context, GPA joins a growing list of autoimmune disorders associated with COVID-19, including systemic lupus erythematosus, rheumatoid arthritis, and autoimmune thyroiditis. Longitudinal studies are needed to better understand the prevalence and mechanisms of these post-COVID autoimmune syndromes and their implications for public health.
Key Takeaways from the Study
-Patient Demographics and Presentation: The case involved a 41-year-old male with symptoms suggestive of both pulmonary and renal involvement, which are classic manifestations of systemic GPA.
-Diagnostic Findings: Elevated inflammatory markers, positive C-ANCA, and HRCT findings confirmed the diagnosis of GPA.
-Therapeutic Approach: The patient’s symptoms improved following a combination of corticosteroids and immunosuppressants, emphasizing the importance of early intervention.
The Path Ahead
While this case provides valuable insights, it also raises critical questions. For instance, could certain individuals be more genetically susceptible to post-COVID autoimmune diseases? How do environmental factors and comorbidities influence the risk of developing GPA? Addressing these questions will require robust research involving larger patient cohorts and long-term follow-up.
In the meantime, healthcare providers must remain vigilant for signs of autoimmune complications in COVID-19 survivors. Public awareness campaigns may also be necessary to educate patients about potential post-COVID symptoms that warrant medical attention.
Conclusion
Granulomatosis with polyangiitis is a rare but life-threatening autoimmune condition that can significantly impact quality of life if left untreated. This case highlights the potential role of SARS-CoV-2 in triggering GPA, underscoring the need for heightened clinical awareness and prompt intervention. The findings also call for further research into the long-term effects of COVID-19, particularly its capacity to induce autoimmune responses.
By enhancing our understanding of these complex interactions, we can improve diagnostic accuracy, refine treatment protocols, and ultimately enhance patient outcomes.
The case study findings were published on a preprint server and are currently being peer reviewed.
https://www.researchsquare.com/article/rs-5550669/v1
For the latest COVID-19 News, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/covid-19-can-cause-an-autoimmune-related-blood-complication-known-as-antiphospholipid-syndrome
https://www.thailandmedical.news/news/covid-19-poses-long-term-risks-for-autoimmune-disorders
https://www.thailandmedical.news/articles/coronavirus