Epstein-Barr Virus - Cancer: Study Finds That Epstein-Barr Virus Contributes To The Oncogenesis Of Mature T-Cell Lymphoproliferative Neoplasms!
Nikhil Prasad Fact checked by:Thailand Medical News Team Sep 16, 2023 1 year, 7 months, 4 days, 3 hours, 45 minutes ago
Epstein-Barr Virus - Cancer: The Epstein-Barr Virus (EBV) is a member of the Herpesviridae family and infects more than 90% of the human population, establishing latent infections in memory B cells. While EBV infections are usually asymptomatic, they can lead to conditions such as infectious mononucleosis (IM) in adolescents and young adults. IM is characterized by the proliferation of EBV-infected B lymphocytes controlled by humoral and cellular immune responses, including activated CD8+ cytotoxic T cells.
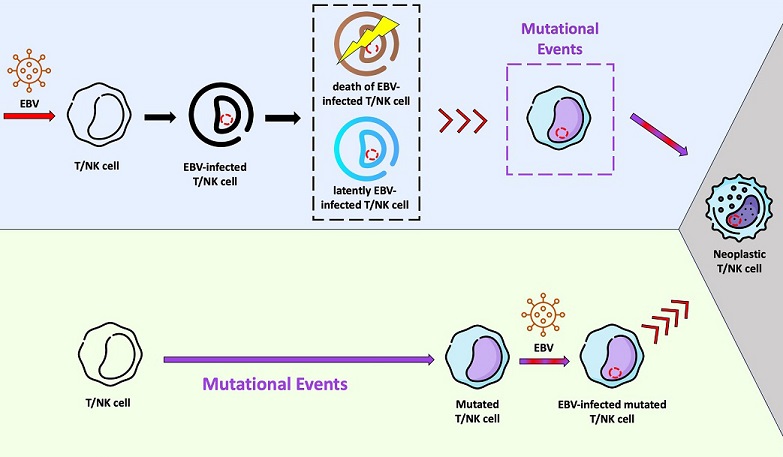
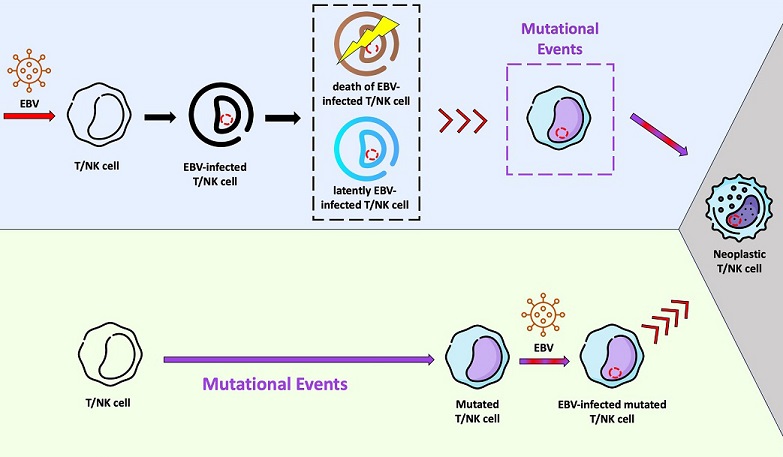 Schematic representation of two hypotheses related with the Epstein-Barr virus (EBV) infection and lymphomagenesis in T/NK cells. In the light purple background, a possible scenario is shown, where EBV infects “healthy” T/NK cells and stablishes a latent infection (cell in blue). It is possible that some of these infected cells are eliminated by the immune system or go into apoptosis (cell in brown). Viral reactivation phases with virus entry into the lytic cycle may occur in infected T/NK cells (red arrows), just as they happen in infected B cells. Mutational events in one EBV-infected T/NK cell may take place later, resulting in the fully malignant phenotype (grey background). In this context, EBV would act as an initiating agent. In the light green background, another hypothesis is presented. The EBV-infection occurs in a previously mutated T/NK cell (initiated cell) and the viral machinery would trigger the fully malignant phenotype (grey background). In this context, EBV would serve as a promoting agent.
Schematic representation of two hypotheses related with the Epstein-Barr virus (EBV) infection and lymphomagenesis in T/NK cells. In the light purple background, a possible scenario is shown, where EBV infects “healthy” T/NK cells and stablishes a latent infection (cell in blue). It is possible that some of these infected cells are eliminated by the immune system or go into apoptosis (cell in brown). Viral reactivation phases with virus entry into the lytic cycle may occur in infected T/NK cells (red arrows), just as they happen in infected B cells. Mutational events in one EBV-infected T/NK cell may take place later, resulting in the fully malignant phenotype (grey background). In this context, EBV would act as an initiating agent. In the light green background, another hypothesis is presented. The EBV-infection occurs in a previously mutated T/NK cell (initiated cell) and the viral machinery would trigger the fully malignant phenotype (grey background). In this context, EBV would serve as a promoting agent.
EBV remains latent in most individuals, but it can reactivate, leading to the release of virions into saliva. This reactivation often occurs when infected memory B cells differentiate into plasma cells. Interestingly, the factors that maintain memory B cell differentiation can also repress lytic activation in EBV.
Despite its ubiquitous presence and generally benign outcomes,
Epstein-Barr Virus - Cancer studies have shown EBV to be etiologically linked to various neoplasms, including nasopharyngeal carcinoma, gastric carcinoma, classical Hodgkin lymphoma, Burkitt lymphoma, post-transplant lymphoproliferative disease, extranodal NK/T-cell lymphoma (ENKTCL), and EBV-positive nodal T- and NK-cell lymphoma (NKTCL). Approximately 200,000 new cases of EBV-associated tumors are diagnosed worldwide each year, leading the International Agency for Research on Cancer (IARC) to classify EBV as a group 1 carcinogen.
While the causal relationship between EBV and B cell lymphomas like Hodgkin and Burkitt lymphomas is well established, the role of EBV in the development of T- and NK-cell lymphoproliferative neoplasms has been less studied. This article explores the contribution of EBV to the oncogenesis of mature T-cell lymphoproliferative neoplasms, focusing on ENKTCL and NKTCL, which exhibit distinctive clinical, histological, and molecular features despite their association with EBV.
EBV Infection of T and NK Cells
Although B cells are the primary target of EBV infection during IM, T and dendritic cells can also become infected, albeit to a lesser extent. CD8+ T cells infected with EBV have been observed, and these in
fected T cells express EBNA1 and EBNA2 proteins, suggesting a latent infection. Studies in healthy individuals and humanized mouse models support the notion that EBV infection alone is insufficient to trigger lymphomagenesis in T/NK cells. Additional events may be necessary for the development of fully malignant phenotypes and the subsequent onset of ENKTCL and NKTCL.
ENKTCL and NKTCL
ENKTCL is an EBV-associated lymphoma that affects either NK or T cells and can manifest in various extranodal sites. This lymphoma has a high prevalence in Asia and South America, suggesting a potential genetic predisposition linked to the host's immune response against EBV.
In contrast, NKTCL predominantly affects T cells and is primarily a nodal lymphoma. It primarily affects elderly or immunocompromised individuals and is associated with B symptoms and advanced stages. NKTCL has recently been recognized as a distinct entity in the WHO classification.
The Role of EBV in Oncogenesis
EBV displays different gene expression profiles depending on the host cell lineage it infects. While B cells are the primary site of EBV infection in IM, the mechanism of infection in T and NK cells is not fully understood. Some studies suggest that T and NK cells may attempt to kill EBV-infected B cells through the immunological synapse, potentially leading to EBV infection in these cells.
The EBV infection mechanism may vary depending on the cell type involved. In vitro studies suggest that EBV-infected T cells exhibit different oncogenic potential compared to EBV-infected B cells. Furthermore, T cells may be more permissive for the expression of immediate early viral genes, potentially contributing to EBV-associated T-cell neoplasms.
EBV's genetic stability can be altered through various mechanisms, including point mutations, deletions, duplications, and homologous recombination. For example, the del30 polymorphism in LMP1 has been associated with different lymphomas worldwide.
EBV in ENKTCL and NKTCL
EBV is present in nearly all cases of both ENKTCL and NKTCL, but the exact latency pattern of the virus remains unclear. Some studies suggest that ENKTCL may exhibit latency I or II, while others propose latency III. High levels of antibodies against specific EBV proteins have been detected in ENKTCL patients, suggesting some degree of viral replication. However, the clinical significance of these findings remains uncertain.
In NKTCL, the majority of cases seem to display latency II, with the expression of EBNA1, BART, LMP1, LMP2A, and LMP2B. Some cases may exhibit latency III with additional EBNA2 expression. The exact pattern of viral latency within neoplastic cells and the proportion of cells in the lytic cycle remain unknown.
Potential Targets for Immunotherapy
Epitopes derived from EBV proteins offer potential targets for immunotherapy in ENKTCL and NKTCL. Adoptive immunotherapy with antigen-specific cytotoxic T cells (CTL) has been explored for EBV-associated tumors and has shown safety and objective responses in ENKTCL cases. LMP1- and LMP2-derived epitopes are considered promising targets for CTL immunotherapy in these lymphomas.
Human Leukocyte Antigens (HLA) in ENKTCL and NKTCL
The host's genetic background, particularly HLA, plays a crucial role in the immune response against EBV and tumor antigens. Different HLA haplotypes are associated with various diseases, including autoimmune disorders and neoplasms. Studies have suggested an association between specific HLA-DRB1 haplotypes and ENKTCL risk.
Conclusions
While ENKTCL and NKTCL are distinct lymphomas with well-established clinical and molecular differences, the role of EBV in their oncogenesis remains enigmatic. EBV can infect T/NK cells, but it is unlikely to be the sole trigger for lymphomagenesis. Additional genetic and immunological factors may be involved in the development of these neoplasms. Understanding the complex interplay between EBV, host genetics, and immune responses in these lymphomas is essential for developing targeted therapies and improving patient outcomes. Further research is needed to unravel the intricacies of EBV-associated T- and NK-cell lymphoproliferative neoplasms.
It should also be noted that with SARS-CoV-2 causing the reactivation of EBV, we can also expect the incidences of various cancers including ENKTCL and NKTCL to increase exponentially!
The study findings were published in the peer reviewed journal: Frontiers in Oncology!
https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2023.1240359/full
For more about
Epstein-Barr Virus - Cancer, keep on logging to Thailand Medical News.