Nikhil Prasad Fact checked by:Thailand Medical News Team Aug 17, 2024 1 year, 4 months, 5 days, 10 hours, 59 minutes ago
Immunology Updates: Taiwanese researchers from Taipei Tzu Chi Hospital, Fu Jen Catholic University, Taoyuan Armed Forces General Hospital, Tri-Service General Hospital, and Ming Chuan University have conducted an in-depth review on the relationship between various types of cell death and host immune pathways. Their findings reveal how these processes work together to defend the body against a wide array of pathogens. This
Immunology Updates news delves into these complex interactions, offering a simplified yet comprehensive understanding of how our immune system utilizes cell death as a key defense mechanism.
 Exploring cell death mechanisms and their crucial role in host immune pathways
The Immune System’s Arsenal: A Multi-Layered Defense Strategy
Exploring cell death mechanisms and their crucial role in host immune pathways
The Immune System’s Arsenal: A Multi-Layered Defense Strategy
The immune system is a highly sophisticated network designed to protect the body from diverse threats, including viruses, bacteria, fungi, and parasites. To achieve this, it employs a variety of immune pathways, each tailored to combat specific types of pathogens. These pathways include TH1, TH2, TH3, TH9, TH17, TH22, TH1-like, and THαβ, each associated with a unique immune response.
TH1 Pathway: This pathway primarily targets intracellular microorganisms, such as bacteria, protozoa, and fungi. It is closely associated with a type of programmed cell death called pyroptosis, which we will discuss in more detail later.
TH2 Pathway: TH2 immunity is directed against multicellular parasites, such as helminths and insects. It often works in tandem with the cell death process of NETosis, which we’ll also explore further.
TH3 Pathway: This pathway deals with viral infections in a more tolerant manner than other immune responses. It is intricately linked with autophagy, a type of cell death that helps manage chronic viral infections.
TH9 Pathway: Similar to TH2, TH9 immunity targets parasites but does so in a more regulated manner, often modulating the immune response to prevent excessive damage to the host.
TH17 Pathway: This pathway focuses on extracellular pathogens and is strongly associated with NETosis, a unique form of cell death employed by neutrophils.
TH22 Pathway: TH22 immunity is geared towards extracellular bacteria, fungi, and protozoa, with a significant role in activating necroptosis, a form of programmed cell death that we’ll cover in detail.
TH1-like Pathway: This pathway is a more regulated version of the TH1 response, using ferroptosis to manage intracellular infections without causing excessive damage to the host.
THαβ Pathway: THαβ immunity is specifically designed to combat viruses and prions, utilizing apoptosis, one of the most well-known forms of cell death,
to destroy infected cells.
Apoptosis: The Precision Strike Against Viruses
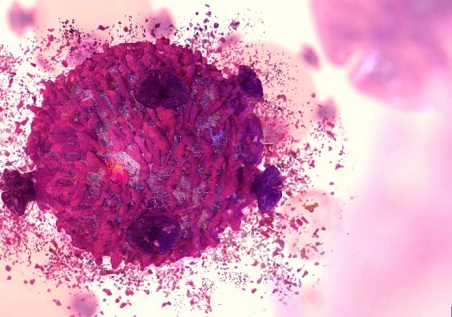
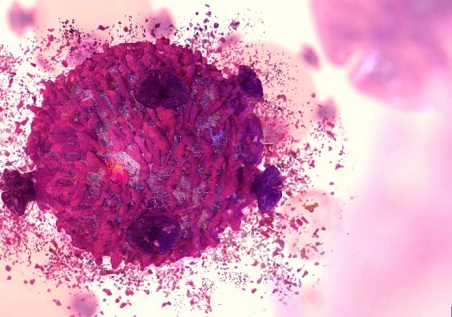
Apoptosis is the most well-studied form of programmed cell death, playing a crucial role in the THαβ immune pathway. This pathway is the body’s primary defense against viruses and prions, which must live inside host cells to replicate. During apoptosis, infected cells are systematically dismantled, with their DNA or RNA fragmented and degraded. This process not only kills the virus-infected cell but also ensures that the viral genome is destroyed, preventing the virus from spreading.
In the context of the THαβ pathway, apoptosis is activated by natural killer (NK) cells and cytotoxic T cells. These immune cells recognize infected cells through specific receptors and initiate the apoptosis machinery, leading to the cell's death. The process involves the activation of caspases, a family of protease enzymes that break down the cell’s components. Apoptosis is a clean and controlled process, with the dying cell neatly packaged into small vesicles that are then consumed by phagocytes, preventing any inflammatory response.
Autophagy: Managing Persistent Viral Threats
Autophagy, another form of programmed cell death, plays a central role in the TH3 immune pathway, which is the body’s response to chronic viral infections. Unlike apoptosis, which is a precise and clean form of cell death, autophagy is more about cellular maintenance and recycling. When a cell is under stress, such as during starvation or viral infection, it activates autophagy to degrade damaged or unnecessary components, including viral particles.
In the TH3 pathway, autophagy helps to contain chronic viral infections by degrading viral particles within specialized structures called autolysosomes. This process is less aggressive than apoptosis and is designed to manage rather than completely eradicate the virus, thus reducing inflammation and potential tissue damage. For example, during a chronic hepatitis C infection, liver cells may use autophagy to degrade viral particles, keeping the infection under control without triggering a full-blown immune response that could damage liver tissue.
Pyroptosis: A Fiery Defense Against Intracellular Invaders
Pyroptosis is a highly inflammatory form of cell death that plays a critical role in the TH1 immune pathway, which targets intracellular bacteria, protozoa, and fungi. This pathway is designed to eliminate these pathogens by sacrificing the infected host cells in a process that involves swelling, bursting, and the release of pro-inflammatory cytokines. The result is a potent immune response that quickly recruits additional immune cells to the site of infection.
The pyroptosis process is driven by the formation of an inflammasome, a complex of proteins that activates caspases responsible for triggering cell death. The key cytokines involved in this process are interleukin-1β and interleukin-18, both of which are released during pyroptosis and help to amplify the immune response. The TH1 pathway is also associated with type 4 delayed-type hypersensitivity reactions, which are part of the body’s defense against persistent intracellular infections.
Ferroptosis: Starving Pathogens of Vital Resources
Ferroptosis is a unique form of cell death associated with the TH1-like immune pathway, which deals with intracellular infections in a more regulated manner. This process is driven by the accumulation of iron and oxidative stress within the cell, leading to lipid peroxidation and membrane damage. Ferroptosis is particularly effective against intracellular bacteria, protozoa, and fungi, as it deprives these pathogens of the iron they need to survive.
In the context of the TH1-like pathway, ferroptosis helps to control chronic infections by eliminating infected cells and the pathogens they contain. This process is tightly regulated by glutathione peroxidase 4 (GPX4), an enzyme that protects cells from lipid peroxidation. When GPX4 is inhibited, cells become more susceptible to ferroptosis, making this pathway a potential target for therapies aimed at controlling chronic infections.
Necroptosis: A Controlled Explosion Against Extracellular Pathogens
Necroptosis is a form of programmed cell death that is similar to necrosis but is tightly regulated by the immune system. This process is closely linked to the TH22 immune pathway, which targets extracellular bacteria, fungi, and protozoa. Necroptosis is triggered by the activation of specific proteins, including TNF-α, RIPK1, and RIPK3, which form a complex known as the necrosome.
The role of necroptosis in the TH22 pathway is to eliminate infected cells while triggering a strong inflammatory response that helps to recruit more immune cells to the site of infection. This process is especially important in acute bacterial infections, where a rapid and potent immune response is required to contain the pathogen. Necroptosis also serves to destroy potential nutrients within the infected cells, depriving extracellular pathogens of the resources they need to survive.
NETosis: The Last Stand of Neutrophils
NETosis is a unique form of cell death that is specific to neutrophils, a type of white blood cell. During NETosis, neutrophils release their DNA to form web-like structures known as neutrophil extracellular traps (NETs), which capture and kill extracellular pathogens such as bacteria, fungi, and protozoa. This process is a key component of the TH17 immune pathway, which deals with persistent extracellular infections.
NETosis is particularly effective in trapping and neutralizing pathogens that have evaded other immune defenses. However, it can also contribute to chronic inflammation and tissue damage if not properly regulated. The TH17 pathway, therefore, carefully balances the benefits of NETosis with its potential harms, ensuring that the immune response is effective without causing excessive damage to the host.
The Immune Pathways in Action
Each of these cell death pathways is intricately linked to specific immune responses, forming a complex network of defenses that the body uses to protect itself from a wide range of pathogens. The TH1, TH2, TH3, TH9, TH17, TH22, TH1-like, and THαβ pathways each play a unique role in this process, with their associated forms of cell death tailored to deal with different types of threats.
TH1 Pathway and Pyroptosis: The TH1 pathway uses pyroptosis to eliminate intracellular pathogens like bacteria and protozoa. This highly inflammatory process ensures that infected cells are rapidly destroyed, preventing the spread of the infection.
TH2 Pathway and NETosis: The TH2 pathway, which targets parasites, often relies on NETosis to trap and kill these large, multicellular invaders. Neutrophils sacrifice themselves to form NETs, which ensnare the parasites and prevent them from causing further harm.
TH3 Pathway and Autophagy: The TH3 pathway deals with chronic viral infections by using autophagy to manage the infection without causing excessive inflammation. This process helps to contain the virus and prevent long-term damage to the host.
TH9 Pathway and Immune Regulation: The TH9 pathway modulates the immune response to parasites, ensuring that the body’s defenses are effective without causing unnecessary damage. This pathway is particularly important in preventing allergic reactions and other hypersensitivities.
TH17 Pathway and NETosis: Like the TH2 pathway, the TH17 pathway uses NETosis to deal with persistent extracellular infections. However, the focus here is on pathogens that are resistant to other forms of immune defense, such as certain bacteria and fungi.
TH22 Pathway and Necroptosis: The TH22 pathway targets extracellular pathogens through necroptosis, a process that destroys infected cells and triggers a strong inflammatory response. This pathway is particularly effective in dealing with acute bacterial infections.
TH1-like Pathway and Ferroptosis: The TH1-like pathway uses ferroptosis to manage intracellular infections in a more regulated manner. This process helps to control chronic infections by depriving pathogens of the iron they need to survive.
THαβ Pathway and Apoptosis: The THαβ pathway uses apoptosis to eliminate virus-infected cells, ensuring that the viral genome is destroyed and preventing the virus from spreading. This process is a key component of the body’s defense against viral infections.
Conclusion
In summary, the various forms of programmed cell death, including apoptosis, autophagy, pyroptosis, ferroptosis, necroptosis, and NETosis, are intricately linked to the body’s immune pathways. These processes play crucial roles in defending against a wide range of pathogens, from viruses to bacteria, fungi, and parasites. By understanding these connections, researchers can develop new strategies to enhance immune responses against infections or modulate them in cases of autoimmune disorders.
The study findings were published in the peer-reviewed journal: Aging.
https://www.aging-us.com/article/206035/text
For the latest
Immunology Updates, keep on logging to Thailand Medical News.
Read Also:
https://www.thailandmedical.news/news/iron-driven-cell-death-could-combat-ebv-linked-tumors
https://www.thailandmedical.news/news/the-role-of-coronavirus-proteins-in-apoptosis-or-cell-death
https://www.thailandmedical.news/news/how-covid-19-causes-cell-death-in-the-airways