Furin Could Be Playing A Key Role In The Pathogenesis Of COVID-19 Associated Neurological Disorders
Nikhil Prasad Fact checked by:Thailand Medical News Team Feb 14, 2024 2 years, 1 week, 6 days, 22 hours, 41 minutes ago
COVID-19 News: The global devastation wrought by the coronavirus disease 2019 (COVID-19) pandemic, caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has left an indelible mark on human health and society. With over 770 million confirmed cases and close to 7 million deaths worldwide, the impact of this viral outbreak has been unparalleled as covered in previous
COVID-19 News coverages. While the pandemic has officially ended, the aftermath continues to affect individuals, with many experiencing lingering medical issues such as long-COVID or post-acute sequelae of SARS-CoV-2 infection (PASC). Notably, neurological disorders have emerged as a significant concern, indicating potential long-term consequences that warrant thorough investigation.
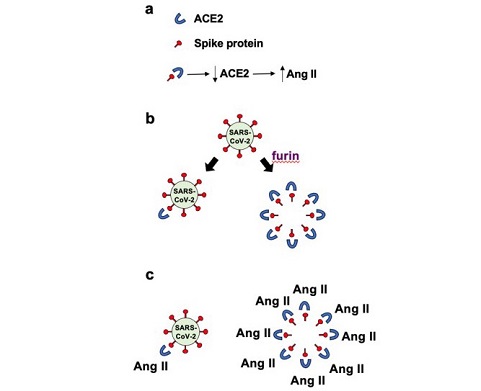
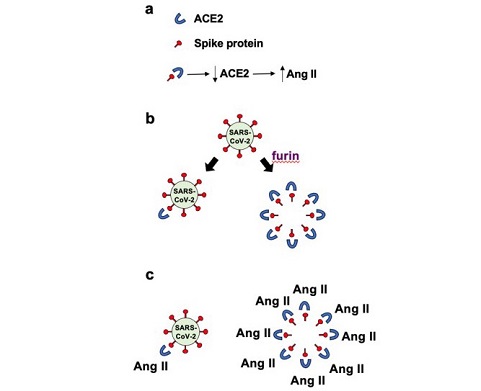 Schemes depicting the main hypothesis of this paper.
Panel a in Figure 1 depicts the binding of the spike protein to ACE2 to downregulate the ACE2 protein. The downregulation of ACE2 results in the reduced overall peptidase activity of this enzyme to degrade Ang II, thereby increasing the levels of Ang II, a major pathogenic mediator. Panel b of
Schemes depicting the main hypothesis of this paper.
Panel a in Figure 1 depicts the binding of the spike protein to ACE2 to downregulate the ACE2 protein. The downregulation of ACE2 results in the reduced overall peptidase activity of this enzyme to degrade Ang II, thereby increasing the levels of Ang II, a major pathogenic mediator. Panel b of
Figure 1 describes that it may be expected that the ratio of roughly one spike protein molecule of one SARS–CoV–2 viral particle interacts with one ACE2 molecule, resulting in downregulating one ACE2 molecule per viral particle. If many spike protein molecules of a given viral particle are cut by the furin protease and come off the virus, multiple (perhaps 50 – 100) free spike protein molecules are produced and can result in the binding of multiple (50 – 100) ACE2 molecules per viral particle. This could result in 50 – 100 ACE2 molecules becoming downregulated. Panel c in Figure 1 describes that the amplification of the ACE2 downregulation by furin–dependent cleavage of the spike protein forming free S1 protein that would then dramatically increase the level of Ang II. Higher levels of Ang II are expected to produce more pathological conditions including neurological damage. We propose that this furin‐dependent amplification process contributes to the mechanism of COVID–19 associated neurological disorders
Understanding SARS-CoV-2 Invasion and Neurological Impacts
Initially perceived as primarily a respiratory illness, emerging evidence has revealed the ability of SARS-CoV-2 to infiltrate the central nervous system, leading to a diverse array of neurological impairments. These range from nonspecific symptoms like confusion, anosmia, and anxiety to severe long-term complications such as cognitive impairments, cerebrovascular diseases, demyelinating pathologies, encephalopathy, and stroke. Neurological consequences have been reported in more than 35.6% of COVID-19 cases, highlighting the urgent need to elucidate the virus's invasion mechanisms and its impact on the central nervous system.
ACE2 and the Renin-Angiotensin System in COVID-19
SARS-CoV-2 enters host cells through the interaction between its spike protein and the host receptor angiotensin-converting enzyme 2 (ACE2). ACE2 plays a critical role in converting the pathogenic angiotensin II (Ang II) into the beneficial angiotensin 1–7 (Ang 1–7). Binding of the spike protein to ACE2 leads to the downregulation of ACE2, resulting in increased levels of Ang II. Elevated Ang II activates the Ang II / Ang II receptor type 1 (AT1R) pathway, contributing to various pathogenic mechanisms, including neurological complications and neurodegeneration.
Furin Protease and Spike Protein Cleavage
The spike protein of SARS-CoV-2 contains a furin protease recognition site, and its cleavage enhances the virus's infectivity. Furin-dependent cleavage occurs between the S1 and S2 subunits of the spike protein, releasing the S1 subunit into the bloodstream. This released S1 subunit, which also binds to and downregulates ACE2, can significantly amplify the ability to downregulate ACE2 and produce Ang II. This amplification mechanism, rather than the infection itself, is proposed as the major driving force behind COVID-19 associated neurological disorders.
Evaluating the Hypothesis
Building upon the viral protein fragment theory of COVID-19 pathogenesis, the hypothesis suggests that the furin protease-dependent cleavage of the SARS-CoV-2 spike protein and the release of circulating S1 subunit protein contribute to neurological disorders seen in COVID-19 patients. Experimental findings demonstrate the detection of circulating S1 protein in COVID-19 patients and vaccine recipients. The amplification effect, potentially 50–100 times greater than intact spike proteins, could result in heightened downregulation of ACE2 and subsequent elevation of Ang II.
Consequences and Implications
The loss of ACE2 function due to SARS-CoV-2 infection leads to increased Ang II levels, contributing to various pathologies. The proposed furin-dependent amplification mechanism raises concerns about its role in neurological disorders. If proven, the hypothesis suggests that furin inhibitors could be a potential avenue for mitigating the adverse effects of COVID-19, especially in patients with neurological complications.
Alzheimer's Disease Connection
A pilot study in Kyiv, Ukraine, indicated early signs of Alzheimer's disease in a subset of COVID-19 patients over 75 years old. Immunohistochemical evaluations of human brains revealed reduced ACE2 expression in COVID-19 patients, suggesting a potential link between the furin-mediated amplification of the spike protein and the development of Alzheimer's disease.
Alternative Perspectives and Concluding Thoughts
While the hypothesis primarily focuses on the spike protein's role in downregulating ACE2 and elevating Ang II, alternative perspectives suggest the spike protein may elicit other biological actions independently of Ang II. The furin-dependent production of free S1 proteins could amplify these actions, possibly contributing to various pathogenic processes.
In conclusion, this hypothesis introduces a novel concept that furin protease-dependent cleavage of the SARS-CoV-2 spike protein and the release of the circulating S1 subunit protein may significantly contribute to the neurological disorders associated with COVID-19. Further research is crucial to validate this hypothesis and explore potential therapeutic interventions, such as furin inhibitors, to mitigate the impact of COVID-19 on neurological health.
The study findings were published on a preprint server and are currently being peer reviewed.
https://www.preprints.org/manuscript/202310.2100/v2
For the latest
COVID-19 News, keep on logging to Thailand Medical News.