Nikhil Prasad Fact checked by:Thailand Medical News Team Jan 06, 2025 9 months, 1 week, 3 days, 15 hours, 38 minutes ago
Medical News: Exploring the Impact of Genes on Long-Term Olfactory Dysfunction
COVID-19 has been notorious for causing a wide range of health issues, even after the initial infection subsides. Among these lingering effects, the loss of the sense of smell, or olfactory dysfunction, has proven to be one of the most perplexing. Researchers from the University of Trieste and the Institute for Maternal and Child Health IRCCS Burlo Garofolo, both in Italy, have delved into the genetic underpinnings of this condition. Their recent study sheds light on why some individuals experience persistent olfactory dysfunction after recovering from mild COVID-19, a condition that can significantly impact their quality of life.
 Genetic Insights into Persistent Loss of Smell After COVID-19
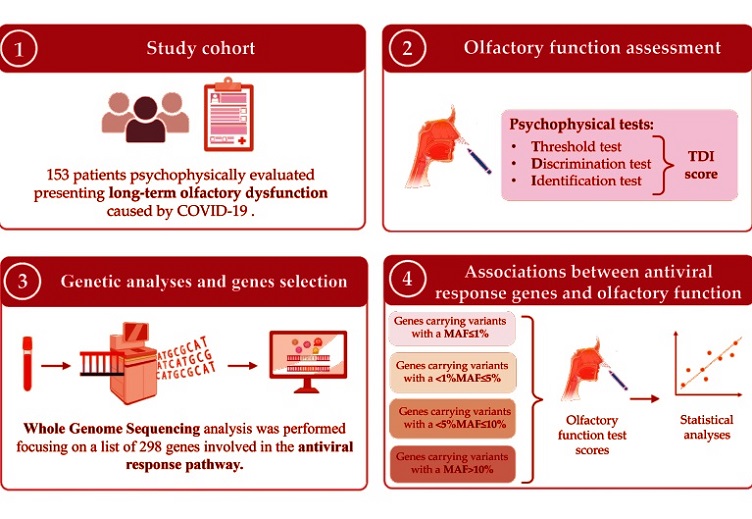
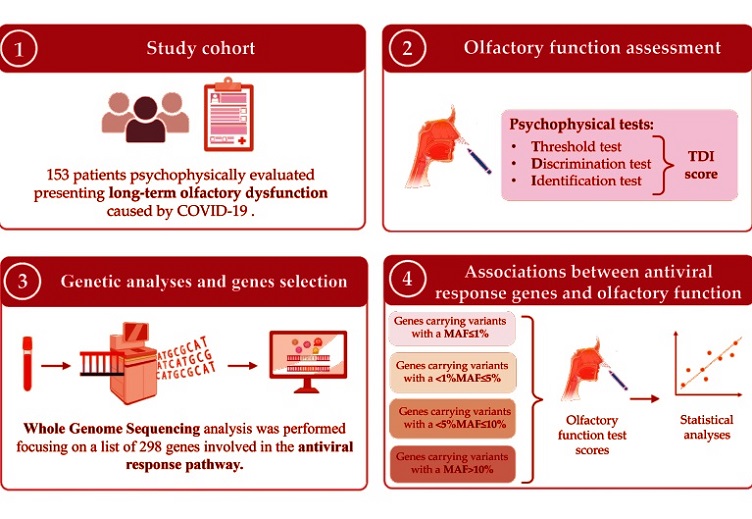
Study workflow. 1. A cohort of 153 patients presenting with persistent post-COVID-19 OD was selected. 2. Olfactory function was psychophysically assessed through the TDI score. 3. WGS analysis was performed, and biallelic variants in 298 genes involved in the antiviral response pathway were extracted. 4. Association analyses between gene score and olfactory performance were performed.
Genetic Insights into Persistent Loss of Smell After COVID-19
Study workflow. 1. A cohort of 153 patients presenting with persistent post-COVID-19 OD was selected. 2. Olfactory function was psychophysically assessed through the TDI score. 3. WGS analysis was performed, and biallelic variants in 298 genes involved in the antiviral response pathway were extracted. 4. Association analyses between gene score and olfactory performance were performed.
This
Medical News report delves into the findings of this research, which utilized whole genome sequencing (WGS) to analyze 153 patients with long-term olfactory dysfunction. By focusing on genetic variants in antiviral response pathways, the researchers aimed to unravel the mystery of why some people’s sense of smell does not fully recover.
Understanding the Scope of the Study
The study involved patients aged 18 and older who reported long-term loss of smell lasting more than three months after mild COVID-19. Mild cases were defined as those without significant respiratory distress or oxygen saturation below 94 percent. Participants underwent psychophysical evaluations using the Sniffin’ Sticks test, which assesses odor thresholds, discrimination, and identification, collectively scored as the TDI (Threshold, Discrimination, Identification) score. A score below 16 indicated anosmia (loss of smell), while scores up to 30.5 indicated hyposmia (reduced smell). Only 12.4 percent of the participants regained normal olfactory function.
Key Genetic Findings
Using WGS data, the researchers examined both rare and common genetic variants in 298 genes linked to antiviral responses. Significant findings included associations between the ACE2 gene and worse olfactory performance, particularly in women, and associations between two other genes, IFI44 and NDUFAF4, with improved olfactory function, especially in men.
ACE2 Gene and Inflammation
The ACE2 gene encodes the Angiotensin-Converting Enzyme 2, which plays a crucial role in regulating inflammation. This gene is also the primary receptor for the SARS-CoV-2 virus. The study found that women with higher numbers of rare genetic variants in ACE2 had worse TDI scores. The researchers hypothesized that these variants might exacerbat
e inflammation in the olfactory epithelium, the area responsible for detecting smells. Prolonged inflammation could impair the regeneration of olfactory neurons, leading to persistent smell loss.
IFI44 and NDUFAF4 Genes
The IFI44 gene is part of the interferon-stimulated gene family, which plays a role in the body’s antiviral response. While IFI44 is known to regulate inflammation, its overexpression could prevent excessive immune reactions, leading to better outcomes. Similarly, the NDUFAF4 gene, which supports mitochondrial function, might help mitigate oxidative stress and inflammation during viral infections. Men with higher levels of common variants in these genes exhibited better olfactory discrimination scores.
Broader Implications of the Findings
Olfactory dysfunction is more than just a sensory inconvenience. It affects nutrition, safety, and mental health. For example, individuals may struggle to detect spoiled food, leading to potential health risks, or feel socially isolated due to their condition. Understanding the genetic basis of persistent olfactory dysfunction could pave the way for targeted treatments. For instance, therapies aimed at reducing inflammation in the olfactory epithelium or supporting neuronal regeneration might emerge as viable solutions.
Conclusions and Future Directions
The findings from this study provide a crucial piece of the puzzle in understanding long-term COVID-19 effects. By identifying specific genetic factors associated with olfactory dysfunction, the research highlights the importance of personalized medicine in addressing long COVID symptoms. Future research could explore larger, more diverse populations to validate these findings and identify additional genetic contributors. Longitudinal studies tracking patients over time could also help determine whether olfactory recovery is possible and what factors influence it.
The study findings were published in the peer-reviewed journal: Life
https://www.mdpi.com/2075-1729/15/1/56
For the latest COVID-19 News, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/folate-deficiency-aggravates-covid-19-impacts-on-brain-health
https://www.thailandmedical.news/news/natural-bioactive-compounds-from-fungi-exhibit-dual-inhibitory-effects-on-sars-cov-2-proteases
https://www.thailandmedical.news/news/the-broad-antiviral-potential-of-the-tcm-decoction-fuzheng-jied-against-various-coronaviruses-including-sars-cov-2
https://www.thailandmedical.news/news/favipiravir-that-was-used-to-treat-covid-19-actually-causes-lung-inflammation-lung-damage-and-lung-fibrosis
https://www.thailandmedical.news/articles/coronavirus