Glaucoma News: American Study Shows That Parvalbumin Expression Decreases With Retinal Ganglion Cell Degeneration
Nikhil Prasad Fact checked by:Thailand Medical News Team Oct 23, 2023 1 year, 5 months, 3 weeks, 4 days, 15 hours, 2 minutes ago
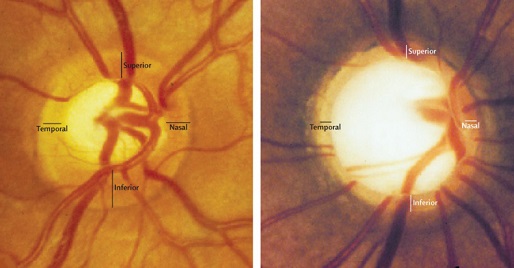
Glaucoma News: Glaucoma, a leading cause of irreversible blindness globally, poses a significant public health challenge. It is estimated that in 2013, 64.3 million people were affected by this disease, with projections suggesting an increase to 76 million in 2020 and a staggering 111.8 million by 2040. Glaucoma encompasses a group of optic neuropathies characterized by the gradual degeneration of retinal ganglion cells (RGCs) and their axons, resulting in visual field defects and, ultimately, blindness. RGCs, found in the innermost layer of the retina, play a pivotal role in transmitting visual information to the brain. As these cells degenerate, the capacity for information transmission is severely compromised, classifying glaucoma as a neurodegenerative disorder.
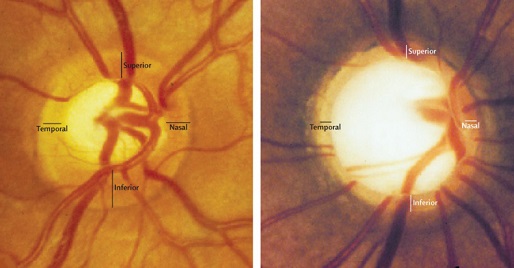
However, the etiology of glaucoma is complex, with multiple theories proposed to explain its pathogenesis and progression. These theories include elevated intraocular pressure (IOP), neurotrophin deprivation, vascular dysregulation, and neuroinflammation. Given this multifaceted nature, identifying biomarkers that enable a more profound understanding of the disease, the monitoring of its progression, and the development of effective treatments is of utmost importance.
This
Glaucoma News report covers a recent study by researchers from the University of Miami Health System-USA, Mount Sinai Hospital, New York-USA and Envision Eye Specialists,-Florida-USA that has found a correlation between parvalbumin expression changes and retinal ganglion cell degeneration.
Parvalbumin (PVALB), a calcium buffer protein, is part of the EF-hand calcium-binding protein family. The EF-hand motif, a helix-loop-helix structure, allows PVALB to bind calcium or magnesium ions, thus regulating intracellular calcium concentrations. This ability to modulate calcium-dependent signaling pathways is crucial for various cellular processes. PVALB was initially discovered in carp muscle, where it played a role in muscle relaxation by shuttling calcium to the sarcoplasmic reticulum. Moreover, PVALB is expressed widely throughout the central and peripheral nervous systems, including the cerebellum, hypothalamus, hippocampus, olfactory bulb, retina, and spinal ganglia. Its abundance and specificity in neurons have led to its use as a neuronal marker, facilitating the differentiation and characterization of neuron subpopulations.
In the mammalian retina, PVALB exhibits immunoreactivity in the inner nuclear layer (INL) and the ganglion cell layer (GCL), labeling amacrine cells and RGCs. In the adult C57BL/6J mouse retina, approximately 85.93% of PVALB-immunoreactive cells were RGCs, and nearly 29% of RGCs expressed PVALB.
Furthermore, PVALB-immunoreactive RGCs displayed morphological heterogeneity, signifying different RGC subpopulations. This study aimed to investigate whether PVALB is a dependable RGC marker in adult mouse eyes and if its expression correlates with progressive RGC loss in glaucoma and optic nerve injury models.
Methods
To explore the role of PVALB in glaucoma, researchers employed the chronic, progressive DBA/2J mouse model of glaucoma and the C57BL6/J optic nerve crush (ONC) mouse model. Various technique
s, such as gene expression microarray analysis, quantitative real-time polymerase chain reaction (qRT-PCR), Western blot, and immunohistochemistry, were used to assess PVALB expression changes with RGC and optic nerve degeneration.
Study Findings
In the DBA/2J mice, PVALB expression exhibited a reduction in response to aging and the development of glaucoma with retinal ganglion cell loss. Microarray analysis of retinal gene expression in these mice revealed decreasing PVALB expression with age. This pattern was further confirmed through qRT-PCR analysis, which demonstrated a significant reduction in PVALB mRNA levels in the retinas and optic nerves of older DBA/2J mice and those subjected to ONC, compared to young DBA/2J mice.
Western blot analysis supported these findings by showing a significant reduction in PVALB protein expression in the retinas and optic nerves of older DBA/2J mice and in eyes following ONC. Immunohistochemical staining results corroborated these findings, showing fewer PVALB-positive cells in the GCL of the retina and altered staining patterns in the optic nerve of older DBA/2J mice and those subjected to ONC.
Parvalbumin expression changes were also observed in the optic nerve, where PVALB immunoreactivity, which colocalized with Tuj-1, a widely-used marker for nerve fibers, diminished in the optic nerves of mice after ONC. qRT-PCR and Western blotting further demonstrated a significant reduction in PVALB expression in crushed optic nerves.
In the DBA/2J mice, PVALB expression changed as they aged and developed glaucoma. Fewer RGCs exhibited immunoreactivity for PVALB in the 14-month-old DBA/2J mice compared to age-matched C57BL6/J mice and young 4-month-old DBA/2J mice. Microarray analysis and qRT-PCR confirmed that PVALB was a potential RGC marker, with its signal intensity decreasing as the mice aged. Furthermore, PVALB expression showed a decrease with the progression of glaucoma in DBA/2J mice.
Implications
This study sheds light on the potential of PVALB as a valuable molecular marker for tracking RGC loss in glaucoma and optic nerve injury models. RGCs express PVALB in both C57BL/6J and DBA/2J mouse strains, a finding consistent with previous research identifying multiple RGC types expressing PVALB in the mouse retina. Crucially, this study demonstrated that PVALB expression decreases with RGC degeneration in the retina and optic nerves, making it a promising marker for tracking RGC loss.
Notably, this reduction in PVALB expression has been previously observed in response to various forms of injury, such as retinal ischemia/reperfusion, ONC, and chronic elevation of IOP. In this study, the decrease in PVALB expression was confirmed in both the retina and optic nerve after ONC. The strong correlation between PVALB and Thy1, a well-established RGC marker, further supports the idea that PVALB can serve as an indicator of RGC degeneration.
This research also delved into the DBA/2J mouse model, a genetic model of glaucoma. The results showed that PVALB expression decreased with age and the progression of glaucoma in these mice, mirroring the timeline of the disease. These findings provide essential insights into the use of PVALB as a marker for tracking glaucoma progression.
The study suggests that PVALB may play a role in modulating calcium signaling within RGCs. Calcium signaling is crucial for neuronal function and survival but can become detrimental when calcium levels are dysregulated or excessive. As a calcium-binding protein, PVALB might assist in regulating calcium levels within RGCs, preventing calcium overload and protecting against degeneration.
The widespread expression of PVALB in RGCs' soma in the mouse retina and their axons in the optic nerve strengthens its potential as a reliable RGC marker for investigating the pathogenesis of various optic neuropathies. This research contributes to the growing body of knowledge about glaucoma and provides a basis for further studies on PVALB's role in neuroprotection within the retina.
Conclusion
Glaucoma is a global health challenge that necessitates the development of reliable markers for its diagnosis, progression monitoring, and treatment. Parvalbumin (PVALB), a calcium-buffering protein, has emerged as a promising marker for tracking retinal ganglion cell (RGC) loss in glaucoma and optic nerve injury models. This study demonstrated that PVALB is abundantly expressed in RGCs in the mouse retina and optic nerves, and its expression decreases with RGC degeneration.
The results of this research have important implications for glaucoma diagnosis and research. The correlation between PVALB and RGC loss provides a valuable tool for studying the pathogenesis of glaucoma and other optic neuropathies. Moreover, the findings highlight the potential role of PVALB in regulating calcium signaling within RGCs, opening new avenues for understanding the mechanisms underlying RGC degeneration.
In summary, the identification of PVALB as a reliable RGC marker is a significant step forward in the quest to better understand and combat glaucoma, offering hope for improved diagnostic accuracy, more personalized treatment strategies, and, ultimately, better outcomes for patients.
The study findings were published in the peer reviewed journal: Frontiers in Neuroscience.
https://www.frontiersin.org/articles/10.3389/fnins.2023.1227116/full
For the latest
Glaucoma News, keep on logging to Thailand Medical News.