Growth Hormone-Releasing Hormone Antagonist MIA-602 Inhibits Inflammation Induced By SARS-CoV-2 Spike Protein In Macrophages And PBMCs
Thailand Medical News Team Aug 16, 2023 1 year, 8 months, 2 days, 2 hours, 14 minutes ago
COVID-19 Research: The global outbreak of coronavirus disease 2019 (COVID-19), caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has led to unprecedented challenges in healthcare systems worldwide. With over 765 million reported cases and 6.9 million deaths globally, the urgency to understand the mechanisms underlying the disease and develop effective therapeutic interventions has never been greater.
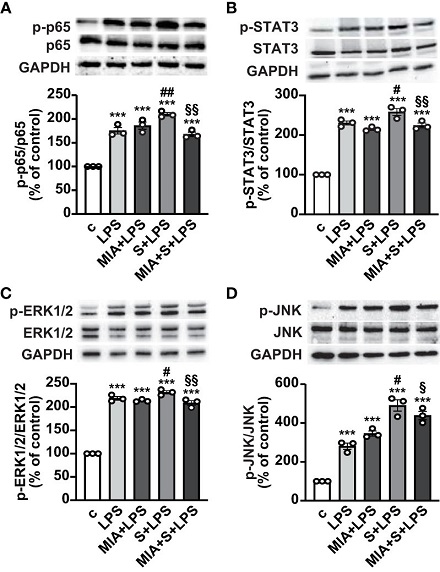
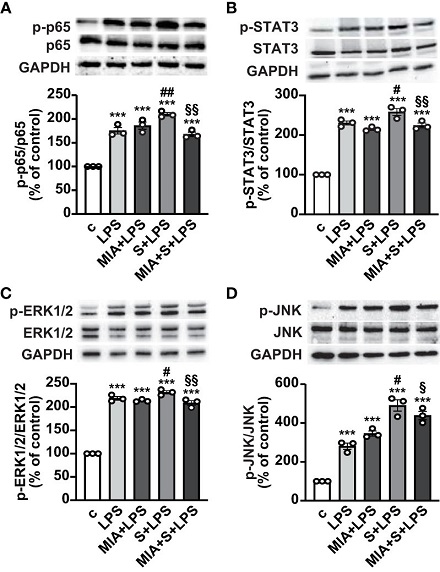 Inhibitory effect of MIA-602 on LPS+S protein-induced activation of inflammatory pathways in THP-1-derived macrophages. Representative Western blots for phosphorylated (p)-p65 (A), p-STAT3 (B), p-ERK1/2 (C) and p-JNK (D) assessed by Western blot in THP-1 cells either untreated (c, control) or pretreated for 3 h with LPS (50 ng/ml), then up to 24 h with either S protein (500 ng/ml), MIA-602 (1 µM) or both (top panel). Blots were reprobed with non-phosphorylated antibodies for normalization (middle panel) or GAPDH, used as internal control (bottom panel). Graphs show the densitometric analysis of phosphorylated proteins normalized to total proteins and reported as percentage of control (means ± SEM). ***P < 0.001 vs. c; #P < 0.05, ##P < 0.01 vs. LPS; §P < 0.05 and §§P < 0.01 vs. LPS+S protein by one-way ANOVA and Tukey’s post-hoc test (n = 3).
Inhibitory effect of MIA-602 on LPS+S protein-induced activation of inflammatory pathways in THP-1-derived macrophages. Representative Western blots for phosphorylated (p)-p65 (A), p-STAT3 (B), p-ERK1/2 (C) and p-JNK (D) assessed by Western blot in THP-1 cells either untreated (c, control) or pretreated for 3 h with LPS (50 ng/ml), then up to 24 h with either S protein (500 ng/ml), MIA-602 (1 µM) or both (top panel). Blots were reprobed with non-phosphorylated antibodies for normalization (middle panel) or GAPDH, used as internal control (bottom panel). Graphs show the densitometric analysis of phosphorylated proteins normalized to total proteins and reported as percentage of control (means ± SEM). ***P < 0.001 vs. c; #P < 0.05, ##P < 0.01 vs. LPS; §P < 0.05 and §§P < 0.01 vs. LPS+S protein by one-way ANOVA and Tukey’s post-hoc test (n = 3).
One of the striking features of COVID-19 is the excessive inflammatory response and hyperactivation of immune cells, particularly macrophages, which can contribute to the development of severe complications such as acute respiratory distress syndrome (ARDS) and multiorgan failure.
Researchers have been working tirelessly to unravel the intricate interactions between the virus and the immune system, with a particular focus on the role of the SARS-CoV-2 spike (S) protein.
The S protein of SARS-CoV-2 plays a crucial role in the virus's ability to infect host cells by binding to the angiotensin-converting enzyme 2 (ACE2) receptor. This engagement triggers a cascade of events that ultimately lead to the entry of the virus into the host cell. However, recent studies have revealed another aspect of the S protein's behavior – its interaction with bacterial lipopolysaccharide (LPS), a potent activator of the immune system. This interaction has been shown to enhance inflammatory responses in immune cells such as macrophages and peripheral blood mononuclear cells (PBMCs).
In light of these findings, a team of researchers from the University of Turin in Italy, the Veterans Affairs Medical Center in Miami, USA, and the University of Miami embarked on a groundbreaking study to investigate a potential therapeutic avenue for mitigating the inflammation induced by the S protein-LPS interaction. Their focus turned to a hormone known as growth hormone-releasing hormone (GHRH), which has previously been implicated in a variety of cellular functions, including cell growth and immune response modulation.
GHRH functions by binding to specific receptors on target cells, promoting the synthesis and release of growth hormone (GH) from the pituitary gland. Notably, GHRH also exerts peripheral effects beyond its role in hormone regulation, making it a versatile player in various physiological and pathological processes.
Moreover, GHRH antagonists have demonstrated potent anti-tumor and anti-inflammatory effects in different cell types, including lung and endothelial cells. However, their potential role in addressing the inflammation associated with COVID-19 had not been explored until now.
The
COVID-19 Research team set out to examine the effects of a specific GHRH antagonist known as MIA-602 on inflammation induced by the S protein-LPS combination in human macrophages (THP-1-derived) and PBMCs. Their comprehensive study revealed several intriguing findings that shed light on the potential therapeutic benefits of GHRH antagonists.
One of the critical observations was the presence of GHRH receptors, including a splice variant known as SV1, in both macrophages and PBMCs. This suggests that GHRH antagonists could effectively interact with these immune cells to modulate inflammatory responses. When exposed to the S protein-LPS combination, THP-1-derived macrophages exhibited increased production of inflammatory cytokines and chemokines, such as TNF-α, IL-1β, IL-8, and MCP-1. Remarkably, the addition of MIA-602 suppressed these responses, indicating its potential to dampen inflammation.
Further investigations into the underlying mechanisms revealed that MIA-602 exerts its anti-inflammatory effects by interfering with key signaling pathways, including NF-κB, STAT3, MAPK ERK1/2, and JNK. These pathways are known to contribute to the activation of immune responses and the release of inflammatory molecules. By inhibiting these pathways, MIA-602 effectively curbed the exaggerated immune response triggered by the S protein-LPS combination.
Importantly, the study extended its focus to PBMCs, another vital component of the immune system. MIA-602 was found to reduce cytokine secretion and oxidative stress in PBMCs exposed to the S protein-LPS combination. Additionally, the antagonist hindered the nuclear translocation and activity of NF-κB, further highlighting its potential to mitigate the inflammatory cascade.
Overall, the research presented in this study has unveiled a novel role for GHRH antagonists, specifically MIA-602, in combating inflammation induced by the SARS-CoV-2 spike protein in macrophages and PBMCs. These findings open the door to potential therapeutic applications of GHRH antagonists in the treatment of inflammatory diseases, including severe cases of COVID-19 and related complications.
The study's implications are far-reaching, offering new avenues for drug development and intervention strategies in the ongoing battle against the COVID-19 pandemic. By targeting the immune system's hyperinflammatory response, GHRH antagonists could provide a much-needed tool to mitigate the severity of the disease and improve patient outcomes.
As the global scientific community continues to investigate the intricate interactions between SARS-CoV-2 and the human immune system, studies like this play a crucial role in uncovering potential therapeutic solutions. With the potential to reshape the landscape of COVID-19 treatment and management, GHRH antagonists represent a promising avenue for addressing the devastating consequences of uncontrolled inflammation in severe cases of the disease. As further research unfolds, the hope is that these findings will pave the way for the development of targeted therapies that can bring relief to patients grappling with the impact of COVID-19 and its associated complications.
The study findings were published in the peer reviewed journal: Frontiers in Immunology.
https://www.frontiersin.org/articles/10.3389/fimmu.2023.1231363/full
For the latest
COVID-19 Research, keep on logging to Thailand Medical News.