Harvard Led Study Confirms That SARS-CoV-2 Coronavirus Infects Blood Monocytes Which In Turn Triggers Inflammation!
Source: SARS-CoV-2 Coronavirus Mar 12, 2021 4 years, 1 month, 6 days, 19 hours, 35 minutes ago
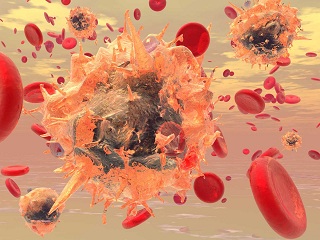
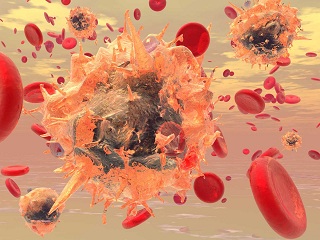
A new study led by researchers from Harvard University Medical School, Boston Children's Hospital and Massachusetts Institute of Technology has alarmingly found that about 10% of blood monocytes in COVID-19 patients are infected with the
SARS-CoV-2 coronavirus. These monocytes subsequently die, leading to the release of cytokines, a feature commonly associated with severe and critical COVID-19.
Often, in certain COVID-19 patients, SARS-CoV-2 infection can lead to acute respiratory distress and multi-organ failure and death.
Also severe disease has been associated with increased pro-inflammatory cytokines and C-reactive protein.
Though severe COVID-19 disease is linked to exuberant inflammation, how SARS-CoV-2 triggers inflammation ito date has not been well understood. Monocytes are sentinel blood cells that sense invasive infection to form inflammasomes that activate caspase-1 and gasdermin D (GSDMD) pores, leading to inflammatory death (pyroptosis) and processing and release of IL-1 family cytokines, potent inflammatory mediators.
The study team found that about 10% of blood monocytes in COVID-19 patients are dying and infected with SARS-CoV-2. Monocyte infection, which depends on antiviral antibodies, activates NLRP3 and AIM2 inflammasomes, caspase-1 and GSDMD cleavage and relocalization. Signs of pyroptosis (IL-1 family cytokines, LDH) in the plasma correlate with development of severe disease. Moreover, expression quantitative trait loci (eQTLs) linked to higher
GSDMD expression increase the risk of severe COVID-19 disease (odds ratio, 1.3, p<0.005).
The study findings suggest that antibody-mediated SARS-CoV-2 infection of monocytes triggers inflammation that contributes to severe COVID-19 disease pathogenesis.
The study findings were published on a preprint server and have yet to be peer reviewed.
https://www.medrxiv.org/content/10.1101/2021.03.06.21252796v1
It has been known that myeloid cells like monocytes, macrophages, and dendritic cells activate the sensors and receptors, called inflammasomes, which induce inflammation in response to infection.
These cells are generally the most important source of inflammatory cytokines. Other pathways like NF-kB activation can also cause severe inflammation.
Scientists have found signs of inflammasomes in the blood of SARS-CoV-2 infected patients. Upon infection, they assemble into large complexes that activate the inflammatory caspase-1, which processes the cytokines interleukin-1 and pore-forming protein GSDMD that damage cell membrane, leading to cell death and inflammatory cytokine release.
However what activates inflammasomes in the monocytes, a type of white blood cells, is a phenomenon that remains unclear. It is possible that they also become infected by SARS-CoV-2. However, monocytes do not express the angiotensin-converting enzyme 2 (ACE2), the SARS-CoV-2 receptor.
The study team isolated mononuclear cells from 19 healthy donors and 22 COVID-19 patients. About 11% of the monocytes in the COVID-19 patients showed signs of membrane damage. This is a large number to detect beca
use dying cells are difficult to detect as the body rapidly eliminates them.
The researchers then analyzed the plasma from the samples and found high levels of specific markers for pyroptosis, a type of cell death, in the COVID-19 patients.
Importantly IL-6, TNFa, several growth factors, and chemokines were very high in COVID-19 patients.
Furthermore the team found higher levels of pyroptosis markers in patients with severe disease compared to those with mild disease.
Detailed immune gene analysis of 4336 severe cases compared with 623,902 control population samples revealed the GSDMD expression quantitative loci were highly associated with respiratory failure.
Significantly two other inflammasome genes, NLRP3 and NLRC4 were also associated with severe COVID-19.
Detailed analysis also revealed that a large proportion of freshly isolated monocytes in COVID-19 patients had higher levels of inflammasome adapters activated caspace-1 and ASC.
The study findings suggest circulating monocytes in COVID-19 patients may die of pyroptosis, releasing inflammatory cytokines and causing a cytokine storm resulting in poor clinical outcomes.
Interestingly about 10% of the monocytes in COVID-19 patients also showed the presence of SARS-CoV-2 nucleocapsid protein and dsDNA, while these were not seen in the blood of healthy donors. Hence, a small portion of the circulating monocytes in COVID-19 patients shows replicating the SARS-CoV-2 virus.
It must be noted that monocyte infection and cell death have not been widely seen before. This may be because many studies use frozen and thawed cells, and dying cells do not survive this process.
Furthermore since it was believed that monocytes do not express ACE2, researchers have not looked closely at whether they may become infected.
The study findings also suggest opsonizing antibodies may play a role in monocyte infection and inflammation.
Past research has seen clinical deterioration coinciding with detection of antibody response against the virus, and antibody-dependent enhancement may be associated with severe disease.
https://pubmed.ncbi.nlm.nih.gov/32317716/
https://pubmed.ncbi.nlm.nih.gov/32659783/
Importantly characterizing the antibodies that are most effective in monocyte infection will be important in identifying monoclonal antibodies for the treatment and identifying if vaccines generate antibodies that cause monocyte infection and inflammation.
The study team also found a one-to-one relation between monocyte infection and caspase-1 activation. However, it is not clear how SARS-CoV-2 infection activated inflammasomes. Some coronaviruses are known to express three ion channel proteins that disrupt ion concentrations and activate NLRP3 and could be a likely mechanism.
Just as important, the observation of plasma biomarkers of pyroptosis in COVID-19 patients and their correlation to severe disease could potentially be used as a diagnostic test for identifying who might develop severe disease.
Also testing approved drugs that inhibit inflammatory cytokines or GSDMD could also be worth investigating.
The study team also stresses that future studies could also look at other infected cells that express GSDMD, as sources of inflammation, such as pneumocytes and macrophages in the lung.
For the lastest
SARS-CoV-2 Coronavirus News, keep on logging to Thailand Medical News.