Nikhil Prasad Fact checked by:Thailand Medical News Team Nov 18, 2024 4 months, 3 weeks, 4 days, 19 hours, 51 minutes ago
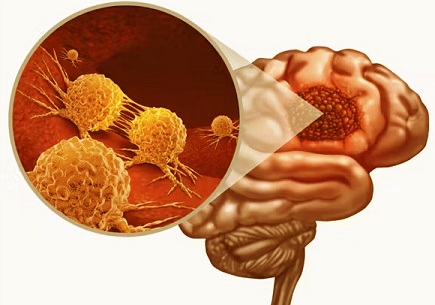
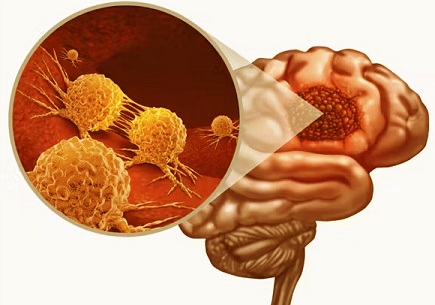
Medical News: A Deadly Challenge in Cancer Treatment
Glioblastoma multiforme (GBM) is a devastating brain tumor with a grim prognosis. Most patients diagnosed with GBM face a survival window of just 15–18 months, as current treatments, including surgery, radiotherapy, and chemotherapy, often fail to prevent recurrence. Despite advancements in cancer research and the initiation of over 2,000 clinical trials, the fight against GBM remains arduous. This
Medical News report delves into recent findings about histone deacetylase 6 (HDAC6) and its potential as a therapeutic target.
 HDAC6 as a Target for Glioblastoma Multiforme Therapy
HDAC6 and Its Role in Glioblastoma
HDAC6 as a Target for Glioblastoma Multiforme Therapy
HDAC6 and Its Role in Glioblastoma
HDAC6, a cytoplasmic enzyme, has emerged as a significant player in GBM. Researchers from Sapienza University in Rome and the National Research Council of Italy have highlighted its role in processes like DNA repair, cellular growth, and resistance to therapies. HDAC6 overexpression in glioblastoma stem cells (GSCs) - a subgroup of cells driving GBM’s aggressiveness and recurrence - makes it a promising target for innovative treatments.
The Complex Biology of HDAC6 in Cancer
HDAC6’s primary functions include deacetylating non-histone proteins like α-tubulin and cortactin, both crucial for cellular architecture and movement. Its ability to regulate protein aggregation, DNA repair, and autophagy allows tumor cells to thrive under stress. In GBM, HDAC6 also interacts with key pathways, including the Sonic Hedgehog (Shh) signaling, contributing to stem cell maintenance and resistance to therapy.
Why Target HDAC6?
GBM’s high intratumoral heterogeneity and immunosuppressive microenvironment complicate treatment. HDAC6 inhibitors (HDAC6i) offer a dual approach: they disrupt critical tumor-supporting pathways and sensitize cancer cells to standard treatments like temozolomide (TMZ) and radiotherapy. Preclinical studies have demonstrated the potential of HDAC6i in reducing tumor cell survival and improving therapeutic outcomes.
Promising Findings from Recent Research
-Primary Cilia and Tumor Progression: HDAC6 influences the formation and function of primary cilia - antenna-like organelles critical for cellular signaling. In GBM, HDAC6-mediated cilia disassembly supports tumor cell proliferation and therapy resistance.
-Resistance Mechanisms: By regulating DNA repair proteins, HDAC6 enhances GBM cells' ability to withstand genotoxic treatments. For instance, it interacts with mismatch repair systems to allow tumor cells to repair chemotherapy-induced DNA damage.
-Tumor Microenvironment: HDAC6 contributes to GBM's interaction with its surrounding microenvironment, aiding in immune evasion and angiogenesis. By stabilizing hypoxia-inducible factor-1α (HIF-1α), it promotes vascular growth, helping tumors survive u
nder oxygen-poor conditions.
-Potential for Drug Development: HDAC6 inhibitors like Tubastatin A and ACY-1215 have shown effectiveness in reducing GBM cell viability and improving responsiveness to other treatments. These inhibitors work by blocking HDAC6’s enzymatic activity, disrupting cellular processes critical for tumor survival.
Challenges in Clinical Translation
While HDAC6i holds promise, challenges like poor blood-brain barrier (BBB) penetration and potential off-target effects need addressing. Innovative drug delivery systems, including nanoparticles, are being explored to improve efficacy and specificity.
Expanding the Horizon: Clinical Implications
The integration of HDAC6-targeting therapies with current GBM treatments could mark a turning point in managing this aggressive cancer. As research progresses, HDAC6’s role in other tumor-supporting pathways and its interaction with immune cells in the tumor microenvironment are gaining attention.
Conclusions
The emerging role of HDAC6 in GBM underscores its potential as a therapeutic target. Its involvement in key tumor-supportive processes like DNA repair, angiogenesis, and cellular resilience makes it a promising focus for drug development. However, translating these findings into clinical practice requires overcoming challenges related to drug delivery and ensuring treatment specificity.
The study findings were published in the peer-reviewed journal: Biomedicines.
https://www.mdpi.com/2227-9059/12/11/2631
For the latest on Glioblastoma Research, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/brain-cancer-study-shows-lumefantrine-enhances-current-protocol-to-treat-glioblastoma-multiforme-gbm
https://www.thailandmedical.news/news/new-combo-therapy-for-glioblastoma
https://www.thailandmedical.news/news/unlocking-the-potential-of-liquid-biopsies-in-glioblastoma-diagnosis-and-treatment
https://www.thailandmedical.news/news/clic4-expression-sheds-light-on-glioma-prognosis-and-immune-response