Hong Kong doctors warn that COVID-19 vaccines can cause severe inflammation of the brain’s blood vessels
Nikhil Prasad Fact checked by:Thailand Medical News Team Jul 25, 2024 9 months, 1 day, 13 hours, 39 minutes ago
Medical News: Recent findings from Hong Kong's top medical institutions have raised concerns over a potential link between COVID-19 vaccines and a severe brain inflammation condition known as cerebral amyloid angiopathy-related inflammation (CAA-ri). Doctors from Queen Mary Hospital-Hong Kong, Tung Wah Hospita-Hong Kong l, and the University of California, San Francisco-USA, have reported a notable case that highlights the importance of understanding the full implications of vaccine-induced immune responses. This
Medical News report delves into the key findings of this study and the broader implications for public health.
 COVID-19 vaccines can cause severe inflammation of the brain’s blood vessels
Understanding Cerebral Amyloid Angiopathy-Related Inflammation
COVID-19 vaccines can cause severe inflammation of the brain’s blood vessels
Understanding Cerebral Amyloid Angiopathy-Related Inflammation
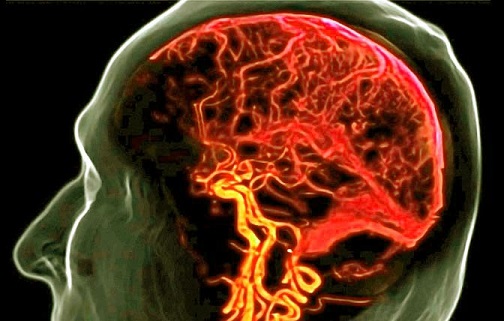
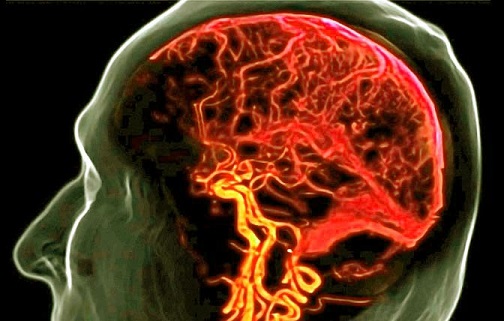
Cerebral amyloid angiopathy-related inflammation (CAA-ri) is a rare but serious condition characterized by inflammation of the brain's blood vessels due to the deposition of amyloid beta proteins. This condition leads to neuroinflammatory changes such as vasogenic edema (fluid leakage into the brain) and microhemorrhages (small brain bleeds), visible on MRI scans. These changes are sometimes referred to as amyloid-related imaging abnormalities (ARIA). Typically, ARIA is associated with anti-amyloid immunotherapy used in Alzheimer's disease treatment, but emerging evidence suggests other triggers may exist.
A Troubling Case of Post-Vaccination
A notable case involved a 67-year-old man who developed severe CAA-ri symptoms 48 hours after receiving his third dose of the inactivated SARS-CoV-2 vaccine (Coronavac). This patient had no significant medical history but began experiencing bradyphrenia (slowed thinking), forgetfulness, and altered behavior. Initial tests, including a CT scan, revealed no abnormalities, but cerebrospinal fluid (CSF) analysis showed signs of inflammation.
A Complex Diagnostic Journey
An urgent MRI revealed faint abnormalities in the left temporal lobe, leading doctors to suspect early meningoencephalitis. Despite treatment with antibiotics and antiviral medication, the patient’s condition deteriorated. Further CSF analysis and MRIs showed worsening inflammation and new brain abnormalities, suggesting an immunological cause. Consequently, doctors administered intravenous immunoglobulin (IVIG), which temporarily improved the patient’s condition.
Challenges and Persistent Symptoms
Despite intensive treatment, including high-dose steroids and additional immunosuppressants, the patient's condition continued to worsen. His MRI scans showed increased inflammation and brain microbleeds. Ultimately, the patient underwent a regime of cyclophosphamide, a potent immunosuppressant, which led to mild improvement. However, significant brain atrophy and complications like chronic osteomyelitis (bone infection) affected his recovery.
Comparing Global Cases
A review of the literature revealed thre
e other reported cases of CAA-ri related to COVID-19 vaccines, all involving different vaccine types. This patient’s case was unique because it was the first linked to an inactivated virus vaccine and exhibited the most robust inflammatory response. This suggests that even less immunogenic vaccines can trigger severe autoimmune reactions in susceptible individuals.
The researchers warn that there could be far more of such cases that were not reported and also in many cases, doctors might misdiagnose the condition.
Possible Mechanisms and Implications
Researchers hypothesize that the overactivation of microglial cells (immune cells in the brain) due to the vaccine’s spike protein might play a role in triggering CAA-ri. The spike protein of SARS-CoV-2 is known to activate microglial inflammasomes, leading to inflammation. This mechanism could explain the immune response observed in this and other cases.
Amyloid PET scans of the patient showed amyloid deposits commonly associated with Alzheimer's disease but not in areas with high CAA-ri activity, supporting the theory that the inflammatory response exceeds the brain’s repair capabilities, leading to severe damage.
Diagnosis and Treatment Complexities
Diagnosing CAA-ri is challenging without a brain biopsy, which was not performed in this case. Clinicians had to rely on clinical signs, symptoms, and MRI features. The lack of standardized terminology and diagnostic criteria further complicates communication and treatment strategies for this condition.
A Call for Caution and Further Research
This case underscores the need for heightened awareness among healthcare providers regarding potential vaccine-induced autoimmune responses. While the benefits of COVID-19 vaccination far outweigh the risks for the general population, understanding and monitoring adverse reactions are crucial for ensuring patient safety.
The study findings and case report were published in the peer-reviewed Journal of Neuroimmunology.
https://www.sciencedirect.com/science/article/abs/pii/S0165572824001255
For the latest
Medical News, keep on logging to Thailand Medical News.
Read Also:
https://www.thailandmedical.news/news/acquired-hemophilia-a-a-rare-side-effect-of-covid-19-vaccines
https://www.thailandmedical.news/news/south-korean-preprint-study-five-months-ago-warns-that-covid-19-mrna-vaccines-can-cause-a-variety-of-blood-disorders-including-aplastic-anemia
https://www.thailandmedical.news/news/doctors-warn-covid-19-mrna-jabs-can-cause-primary-cutaneous-cd4-small-medium-t-cell-lymphoproliferative-disorders-and-cutaneous-lymphomas
https://www.thailandmedical.news/news/covid-19-vaccines-causes-persistence-of-spike-protein-in-the-cd16-monocytes-and-makes-sars-cov-2-negative-people-sick-with-pasc-like-sickness