Hong Kong Study Finds That Benign Prostatic Hyperplasia Patients Suffer From Up To Five Times The Risk Of Urological Complications After COVID-19
Nikhil Prasad Fact checked by:Thailand Medical News Team May 08, 2024 11 months, 2 weeks, 3 days, 47 minutes ago
COVID-19 News: Benign Prostatic Hyperplasia (BPH) is a common condition affecting the male population, particularly those in middle age and older. It involves the non-malignant enlargement of the prostate gland, leading to various urinary symptoms. The prostate, a walnut-sized gland located below the bladder, plays a crucial role in male reproductive function by producing a fluid that nourishes and transports sperm during ejaculation.
 Benign Prostatic Hyperplasia Patients Suffer From Up To Five Times The Risk Of Urological Complications After COVID-19
Benign Prostatic Hyperplasia Patients Suffer From Up To Five Times The Risk Of Urological Complications After COVID-19
As men age, hormonal changes, particularly an increase in dihydrotestosterone (DHT), contribute to prostate growth. This growth can gradually compress the urethra, the tube that carries urine from the bladder out of the body, leading to symptoms such as:
-Urinary Frequency and Urgency: Patients may experience the need to urinate more frequently, especially at night (nocturia), and a sense of urgency when the urge to urinate arises.
-Weak Urine Stream: The flow of urine may become weaker or interrupted, making it challenging to empty the bladder completely.
-Difficulty Initiating Urination: Patients may have trouble starting the urine stream, requiring straining or pushing to begin urination.
-Incomplete Emptying: Despite urinating, patients may feel that their bladder is not completely empty, leading to a sensation of fullness or discomfort.
-Urinary Retention: In severe cases, BPH can cause urinary retention, where the bladder cannot empty properly, leading to pain and potential complications.
Apart from these urinary symptoms, BPH can also lead to complications such as urinary tract infections (UTIs), haematuria (blood in urine), bladder stones, and even kidney damage if left untreated. These complications not only impact a patient's quality of life but can also necessitate medical interventions ranging from medications to surgical procedures.
The Impact of COVID-19 on BPH Patients
The emergence of the COVID-19 pandemic has brought to light the virus's multi-systemic effects beyond respiratory symptoms. Studies have shown that SARS-CoV-2, the virus responsible for COVID-19, can affect various organs and systems, including the urinary system.
Research conducted by the Chinese University of Hong Kong's Faculty of Medicine that is covered in this
COVID-19 News report, has delved into the intersection of COVID-19 and BPH. By analyzing data from a significant cohort of BPH patients within the local public healthcare system, researchers uncovered alarming trends regarding the risks faced by BPH patients infected with COVID-19.
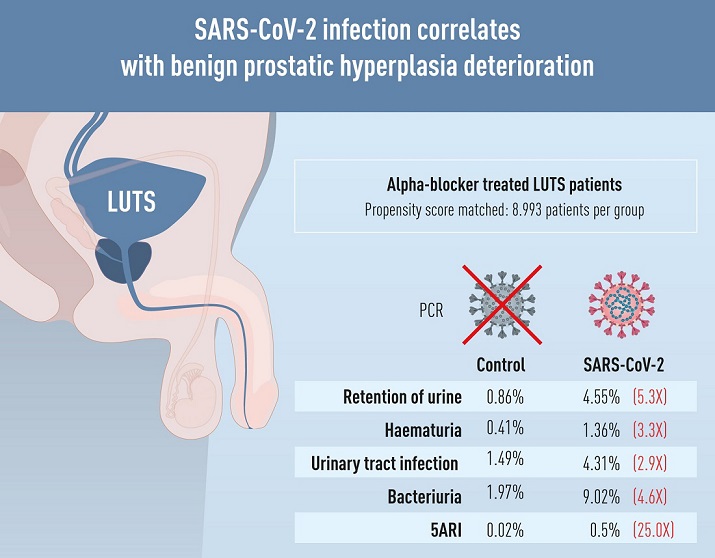
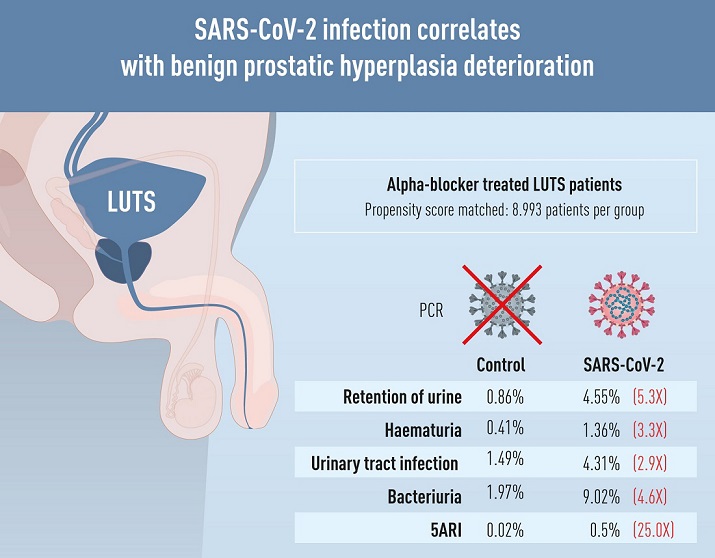
The study examined data from approximately 18,000 BPH patients. Among those infected with COVID-19, t
he incidence rates of complications were found to be 2.9 to 5.31 times higher compared to BPH patients without COVID-19 infection. These complications included urinary retention, bacteriuria (bacteria in urine), haematuria, and the need for combination therapy to manage worsening symptoms post-infection.
The Biological Basis of Complications
Understanding the biological mechanisms underlying these complications is crucial in comprehending why BPH patients are at heightened risk after COVID-19 infection. The prostate gland, like other organs, expresses angiotensin-converting enzyme 2 (ACE2) receptors, which serve as entry points for the SARS-CoV-2 virus. This viral entry into prostate cells can trigger inflammatory responses and disrupt normal cellular functions.
Moreover, COVID-19 has been associated with metabolic dysregulation, including disturbances in glucose metabolism and insulin sensitivity. These metabolic changes can exacerbate existing conditions like BPH, potentially leading to more severe symptoms and complications.
Clinical Implications and Management Strategies
The findings from this study have significant clinical implications for healthcare providers managing BPH patients, especially in the context of the ongoing COVID-19 pandemic. Clinicians need to be vigilant about the increased risks of urinary complications in BPH patients who have been infected with SARS-CoV-2.
Management strategies may involve:
-Regular Monitoring: Close monitoring of BPH patients, especially those with a history of COVID-19 infection, to promptly identify and address any emerging urinary symptoms or complications.
-Optimizing Treatment: Adjusting medication regimens and treatment plans to manage symptoms effectively and prevent acute exacerbations or complications.
-Patient Education: Educating patients about the potential risks and warning signs of urinary complications post-COVID-19 infection, empowering them to seek timely medical attention.
-Collaborative Care: Facilitating multidisciplinary care involving urologists, infectious disease specialists, and primary care providers to ensure comprehensive management and timely interventions.
Challenges and Future Directions
While this study provides valuable insights, several challenges and areas for future research remain. Long-term follow-up studies are needed to assess the persistent effects of COVID-19 on BPH patients and their urinary health. Additionally, exploring the impact of COVID-19 variants and vaccination status on BPH outcomes could further enhance our understanding of these complex interactions.
In conclusion, the COVID-19 pandemic has highlighted the intricate interplay between viral infections like SARS-CoV-2 and pre-existing health conditions such as BPH. By unraveling these connections and implementing proactive management strategies, healthcare providers can optimize care and improve outcomes for BPH patients during these challenging times.
The study findings were published in the peer reviewed Journal of Internal Medicine.
https://onlinelibrary.wiley.com/doi/10.1111/joim.13719
For the latest
COVID-19 News, keep on logging to Thailand Medical News.