Nikhil Prasad Fact checked by:Thailand Medical News Team Jan 23, 2025 11 months, 2 days, 4 hours, 50 minutes ago
Medical News: Sepsis, a life-threatening condition caused by an extreme response to infection, has been a topic of medical inquiry for centuries. Despite advancements in treatment, it remains a leading cause of mortality in hospitals globally. Researchers from The Feinstein Institutes for Medical Research at Northwell Health, the Icahn School of Medicine at Mount Sinai, and Azevan Pharmaceuticals in USA, have delved into the intricate relationship between sepsis and its impact on hormonal and metabolic systems. This
Medical News report outlines their findings, presenting a comprehensive view of how systemic inflammation disrupts bodily functions.
 Hormonal and Metabolic Changes in Response to Inflammation and Sepsis
Sepsis and Its Endocrine Impact
Hormonal and Metabolic Changes in Response to Inflammation and Sepsis
Sepsis and Its Endocrine Impact
Sepsis triggers systemic inflammation, disrupting the body's delicate hormonal balance. This condition, historically described by figures such as Hippocrates, is now recognized as "life-threatening organ dysfunction caused by a dysregulated host response to infection." The body's response to sepsis includes metabolic shifts and hormonal changes that aim to fight infection but often exacerbate organ damage.
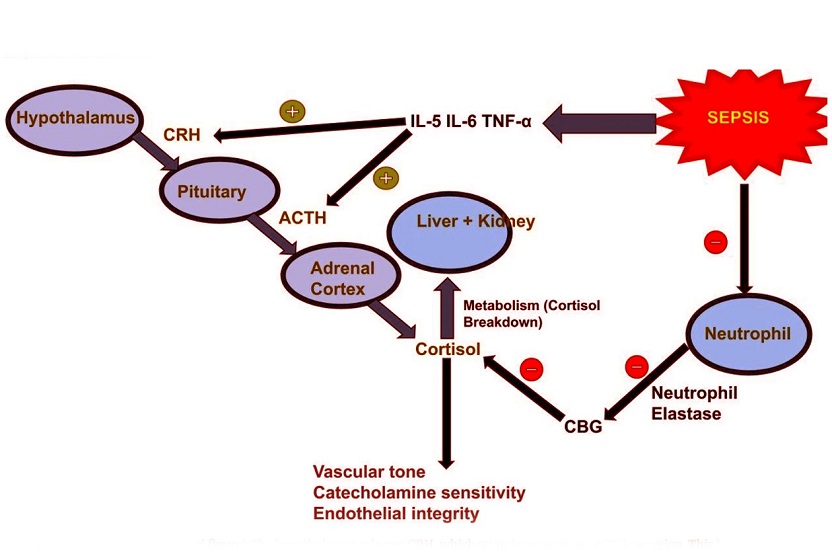
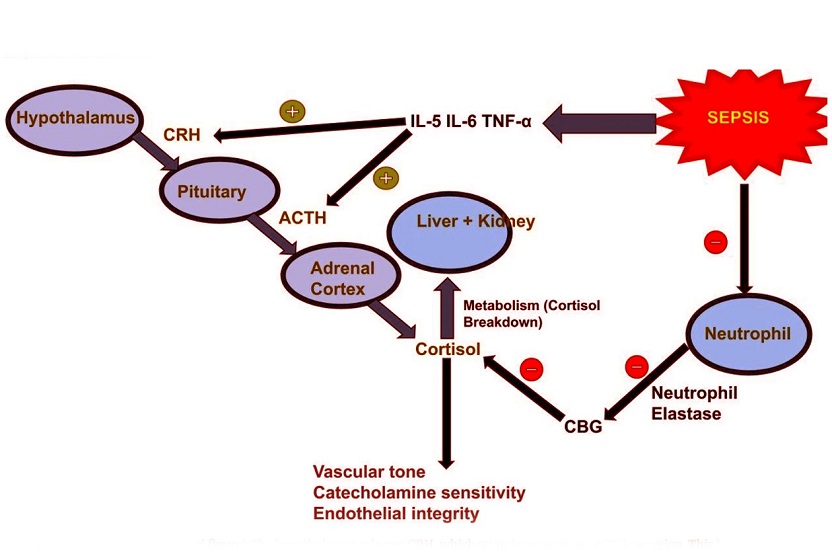
The hypothalamic-pituitary-adrenal (HPA) axis, critical for stress response, becomes overactive during acute sepsis. Increased cortisol levels, while beneficial for vascular tone and immune modulation, can lead to harmful effects such as muscle wasting and impaired glucose metabolism when elevated for prolonged periods. Chronic sepsis, on the other hand, shows desensitization of the HPA axis, resulting in inadequate cortisol production.
The Hypothalamic-Pituitary-Thyroid (HPT) Axis in Sepsis
Thyroid function is particularly vulnerable in septic patients. The study found that many patients exhibit euthyroid sick syndrome (ESS), where triiodothyronine (T3) levels drop significantly, disrupting energy metabolism. The acute phase of sepsis suppresses the enzyme responsible for converting thyroxine (T4) to T3, leading to energy conservation at the expense of overall metabolic efficiency. Over time, chronic inflammation further diminishes thyroid function, affecting patient recovery.
Metabolic Alterations: The Role of Glucose and Insulin
Sepsis causes notable changes in glucose metabolism. Early in the condition, patients may experience stress-induced hyperglycemia, even without a history of diabetes. This phenomenon is attributed to increased cortisol and catecholamine levels. The immune response to sepsis also promotes insulin resistance, complicating glucose regulation. Elevated blood glucose levels provide energy to immune cells but exacerbate tissue damage if left uncontrolled.
Despite initial enthusiasm for intensive insulin therapy in septic patients, recent studies suggest that moderate glucose control yields better outcomes. The Normoglycemia in Intensive Care Evaluation - Survival Using Glucose Algorithm Regulation (NICE-SUGAR) trial recommended targeting blood glucose levels between 140 and 180 mg/dL to reduce mortality and minimize hypoglycemi
a risk.
Growth Hormone and Immune Function
Growth hormone (GH) and insulin-like growth factor 1 (IGF-1) are critical for cellular repair and immune modulation. In sepsis, inflammatory cytokines such as interleukin-1 beta and tumor necrosis factor-alpha suppress IGF-1 production, leading to GH resistance. This shift results in catabolic effects, such as muscle breakdown, further weakening the patient. GH levels tend to correlate with sepsis severity, offering a potential biomarker for disease progression.
Other Hormonal Pathways: Ghrelin and Leptin
Ghrelin, known as the hunger hormone, increases during sepsis and plays a protective role by reducing inflammation. Patients with higher ghrelin levels often exhibit better outcomes, including shorter ICU stays and reduced need for mechanical ventilation. Conversely, leptin, which regulates energy balance, shows a biphasic response in sepsis - initially rising during acute inflammation and then declining in chronic stages. These fluctuations highlight the complex interplay between hormones and immune responses.
The Renin-Angiotensin-Aldosterone System (RAAS) and Sepsis
The RAAS, which regulates blood pressure and fluid balance, becomes overactivated during sepsis. Elevated levels of angiotensin II contribute to vasoconstriction, inflammation, and kidney injury. While RAAS inhibitors such as ACE inhibitors and angiotensin receptor blockers (ARBs) show promise in reducing sepsis-related complications, their impact on blood pressure warrants caution. Researchers advocate for further trials to assess the benefits and risks of these therapies in septic patients.
Conclusions
The findings underscore the profound effects of sepsis on the endocrine and metabolic systems. From thyroid dysfunction to insulin resistance and altered cortisol dynamics, sepsis disrupts homeostasis in ways that influence patient outcomes. Understanding these mechanisms can aid in developing targeted therapies to mitigate organ damage and improve survival rates. Key insights include:
-The importance of moderate glucose control to balance energy needs and minimize complications.
-The protective role of hormones like ghrelin in reducing inflammation and supporting recovery.
-The potential of biomarkers such as IGF-1 and angiotensin II to predict sepsis severity and guide treatment.
Future research should focus on personalized interventions that address the unique hormonal and metabolic needs of septic patients. By integrating these findings into clinical practice, healthcare providers can enhance the management of this complex condition.
The study findings were published in the peer-reviewed journal: Molecular Medicine.
https://link.springer.com/article/10.1186/s10020-025-01074-z
For the latest on Sepsis, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/viral-sepsis-challenges-and-new-insights
https://www.thailandmedical.news/news/phytochemicals-as-potential-saviors-against-covid-19-associated-sepsis
https://www.thailandmedical.news/articles/sepsis