Nikhil Prasad Fact checked by:Thailand Medical News Team Nov 03, 2024 1 year, 2 months, 2 weeks, 1 day, 1 hour, 53 minutes ago
Medical News: CD59 Protein -The “Protector” of Cancer Cells
A new study by researchers from Texas Tech University Health Science Center and the Masonic Cancer Center at the University of Minnesota-USA has shed light on the role of CD59, a protein that helps cancer cells avoid immune attacks. This study, which analyzed data from various sources and experiments, provides insight into how CD59 contributes to cancer progression and influences patient survival across different types of cancer.
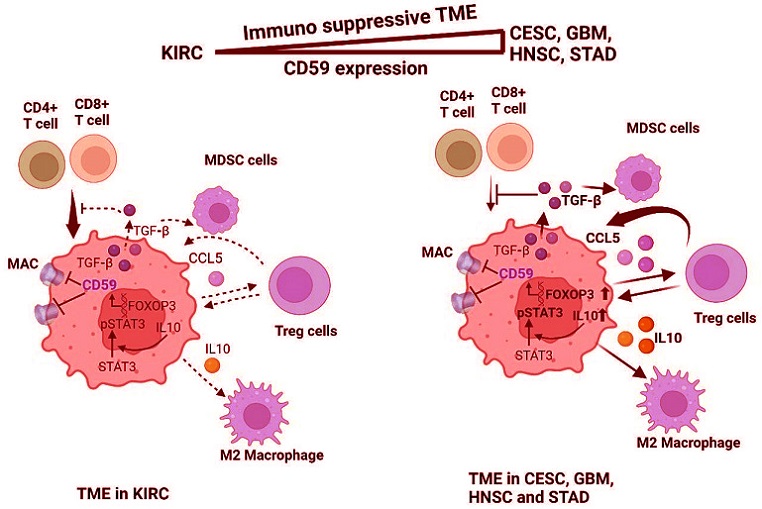
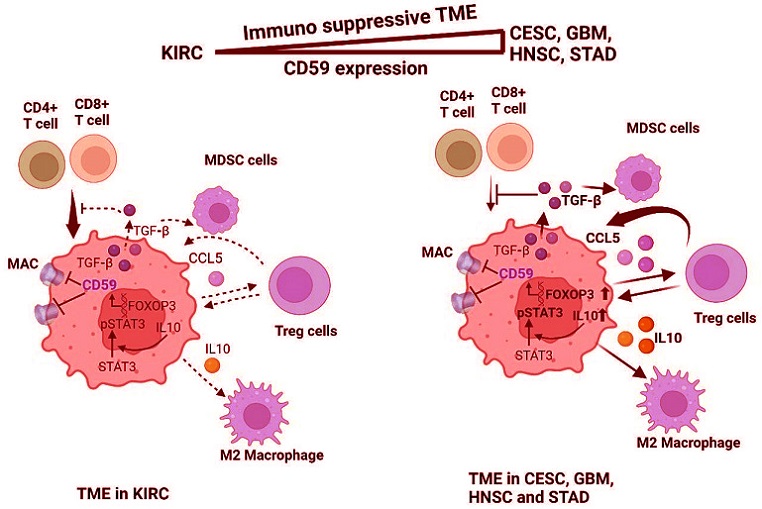 Diagram of CD59-mediated immune suppression in CESC, GBM, HNSC, and STAD. CESC, GBM, HNSC, and STAD have high amounts of FOXP3, IL10, TGFβ1, and pSTAT3, leading to increased CD59 transcription and the recruitment of immune suppressive cells such as MDSC, Treg, and TAM in the TME
How CD59 Shields Cancer Cells from the Immune System
Diagram of CD59-mediated immune suppression in CESC, GBM, HNSC, and STAD. CESC, GBM, HNSC, and STAD have high amounts of FOXP3, IL10, TGFβ1, and pSTAT3, leading to increased CD59 transcription and the recruitment of immune suppressive cells such as MDSC, Treg, and TAM in the TME
How CD59 Shields Cancer Cells from the Immune System
CD59 is a protein found on the surface of cells. It plays a role in blocking the formation of a structure called the membrane attack complex (MAC), which is part of the body’s natural defense against disease. Normally, MAC attacks and breaks down harmful cells, including cancerous ones. However, in many cancer cells, CD59 is overexpressed, meaning there’s more of it present on these cells than usual. This overabundance of CD59 acts as a shield, preventing MAC from doing its job.
This study covered in this
Medical News article, reports that high levels of CD59 in various cancers, such as cervical, brain, head and neck, and stomach cancers, are linked to worse patient outcomes, as it creates an environment where immune cells struggle to attack and eliminate tumor cells. Conversely, in kidney cancer, CD59 expression does not seem to interfere with immune responses, leading to better survival rates for patients.
Understanding the Immune Microenvironment
The researchers also studied how CD59 interacts with immune cells within the tumor microenvironment. Tumors do not exist in isolation; they are surrounded by immune cells that can either support or suppress the body’s ability to fight cancer. The study found that CD59 is particularly active in creating an immune-suppressive environment by associating with certain immune cells, such as T-regulatory cells, myeloid-derived suppressor cells (MDSCs), and macrophages, which contribute to a protective barrier for the tumor.
In particular, the study found that cancers like cervical and brain cancers have higher CD59 activity and are associated with immune-suppressive cells, creating a more challenging situation for the immune system to fight these tumors.
Key Findings on CD59’s Impact on Patient Prognosis
The research team conducted a detailed analysis of CD59 levels across several cancer types. By using databases like The Cancer Genome Atlas (TCGA), they observed a strong link between CD59 levels and patient survival rates. In cancers such as cervical, brain, and stomach, high CD59 levels correlated with shorter survival times and worse prognosis. However, in kidney cancer, where CD5
9 levels do not seem to interfere with immune cell function, patients had better survival outcomes.
Immune Suppression by Recruiting Specific Cells
Further, the study investigated how CD59 attracts immune-suppressive cells into the tumor environment. In cancers with high CD59 levels, such as cervical and stomach cancers, researchers observed an increase in T-regulatory cells and MDSCs, which are known to dampen the immune response. This effect makes it easier for the tumor to grow without being attacked by the body’s immune system.
In addition, CD59’s association with M2 macrophages, a type of immune cell that can suppress other immune cells, was stronger in cancers like cervical and stomach cancers than in kidney cancer. The research shows that CD59 attracts these macrophages to the tumor, helping it escape immune attacks and resist treatments.
Interplay with Other Proteins: The Role of TGF-β1
The researchers also explored how CD59 works alongside another protein, TGF-β1, in promoting immune suppression in the tumor environment. TGF-β1 is a powerful immune-suppressing protein that can enhance CD59’s effects, especially in cancers like cervical and brain cancers. In these cancers, the combination of CD59 and TGF-β1 was linked to a more hostile environment for the immune system, reducing the ability of immune cells to attack and destroy cancer cells.
Interestingly, kidney cancer, which had lower levels of TGF-β1 in this study, did not show the same degree of immune suppression, highlighting why patients with kidney cancer may have better survival rates when CD59 levels are high.
Why CD59 Levels Matter in Cancer Prognosis
The findings indicate that assessing CD59 levels in patients could provide crucial information for predicting outcomes in different cancers. Cancers with high CD59 and TGF-β1 levels may require different therapeutic approaches than those with low levels of these proteins. This insight could lead to more targeted therapies aimed at lowering CD59 activity in tumors, potentially enhancing the effectiveness of immune-based treatments.
Potential for New Cancer Treatments Targeting CD59
The study’s conclusions suggest that therapies targeting CD59 might offer new hope for patients with cancers that currently have poor survival rates. By disrupting CD59’s protective shield, new treatments could potentially make it easier for the immune system to attack cancer cells. In addition, understanding how CD59 works with immune-suppressing cells in the tumor microenvironment may allow for more precise and effective cancer treatments.
Conclusion
Overall, this research highlights the role of CD59 as a key player in immune evasion across various cancers. By examining the unique interactions between CD59 and immune-suppressive cells in different cancers, the study underscores the importance of considering CD59 levels as part of cancer diagnosis and treatment planning. These findings not only expand our understanding of how cancer cells evade the immune system but also open new avenues for developing therapies that could improve patient outcomes in difficult-to-treat cancers. While CD59 helps tumors evade immune attacks, cancers like kidney cancer with fewer interactions between CD59 and immune-suppressive cells show that prognosis varies based on the tumor microenvironment. Future research and clinical trials focusing on CD59 could lead to more effective cancer treatments and better survival rates for many patients.
The study findings were published in the peer-reviewed journal: Cancers.
https://www.mdpi.com/2072-6694/16/21/3699
For the latest Cancer News, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/new-epigenetic-hallmarks-of-cancer-unveiled
https://www.thailandmedical.news/news/glioblastoma-may-weaken-key-immune-cells
https://www.thailandmedical.news/news/selenium-s-potential-in-fighting-carcinogenesis