Nikhil Prasad Fact checked by:Thailand Medical News Team Jan 21, 2025 10 months, 4 weeks, 1 day, 10 hours, 12 minutes ago
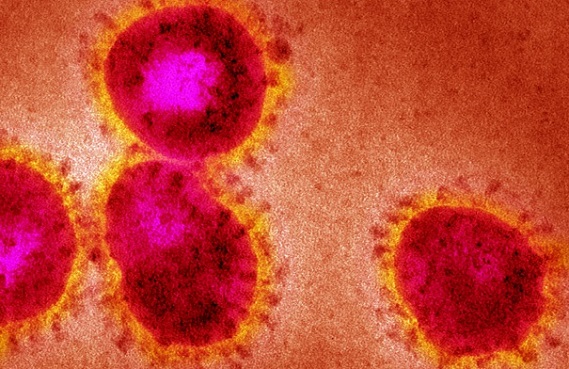
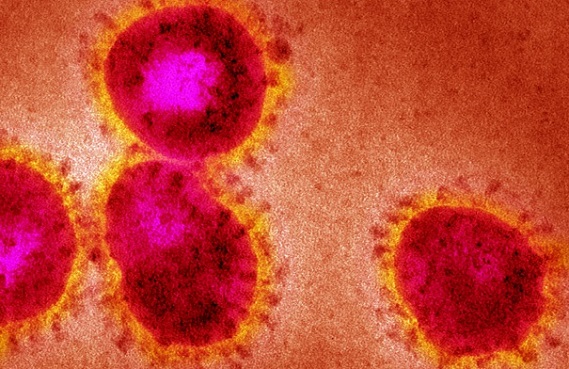
Medical News: The global COVID-19 pandemic, caused by SARS-CoV-2, has brought an urgent need to understand how our immune system responds to the virus. Researchers from the University of Ljubljana’s Biotechnical Faculty in Slovenia conducted a groundbreaking study focusing on the role of Toll-like receptor 10 (TLR10), a less-known player in our immune system, in regulating immune responses during SARS-CoV-2 infection. The findings from this
Medical News report offer a new perspective on combating severe inflammation in COVID-19 patients.
 How TLR10 Modulates Immune Responses to SARS-CoV-2 in Lung Cells
How TLR10 Modulates Immune Responses to SARS-CoV-2 in Lung Cells
Toll-like receptors (TLRs) are essential components of our innate immune system, helping the body recognize and respond to viral infections. Among these, TLR10 stands out as the least understood. This study explored how overexpression of TLR10 in A549 lung epithelial cells influenced the immune response to SARS-CoV-2 structural proteins, spike (S) and nucleocapsid (N).
The Study Design and Methods
The researchers utilized advanced CRISPR/dCas9 technology to overexpress TLR10 in A549 lung epithelial cells. These modified cells were then exposed to SARS-CoV-2 S and N proteins to mimic viral infection. Additionally, co-culture experiments with THP-1 monocytes allowed scientists to examine how TLR10 expression in lung cells affected immune signaling in nearby immune cells.
Key techniques included:
-Real-time PCR and qPCR arrays: To analyze gene expression.
-ELISA assays: To measure levels of cytokines like IL6, IL8, and CXCL10 in cell culture media.
-Western blot analysis: To confirm TLR10 protein levels.
Results: How TLR10 Affects Immune Responses
Overexpressing TLR10 significantly altered the immune responses in A549 cells when exposed to SARS-CoV-2 proteins. Key findings include:
-Reduction of Proinflammatory Cytokines: The overexpression of TLR10 reduced the production of inflammatory markers such as CXCL10, IL6, IL8, and interferon-β (IFNβ). These markers are typically elevated in severe COVID-19 cases and contribute to hyperinflammation or "cytokine storms."
-Temporal Effects: The impact of TLR10 was more pronounced at early stages (four hours) of immune stimulation, with effects diminishing by 24 hours.
-Co-Culture Insights: In experiments involving THP-1 monocytes, TLR10 overexpression in lung epithelial cells influenced nearby immune cells. The monocytes displayed reduced levels of proinflammatory cytokines after exposure to SARS-CoV-2 proteins.
Potential Therapeutic Implications
One of the most promising aspects of the study is the potential for TLR10 to serve as a therapeutic target. The researchers noted that excessive inflammation during severe COVID-19 can lead to acute respiratory distress syndrome (ARDS
). By modulating TLR10 activity, it might be possible to control this harmful inflammation without suppressing the overall immune response.
Interestingly, the study also explored the role of vitamin D. Adding active vitamin D to the cell culture significantly increased TLR10 expression. This finding aligns with earlier evidence suggesting that vitamin D can support immune health during respiratory infections, including COVID-19.
Study Conclusions
The study offers compelling evidence that TLR10 plays a critical role in controlling the immune response to SARS-CoV-2 proteins. Overexpression of TLR10 was shown to:
-Downregulate harmful proinflammatory cytokines and chemokines.
-Potentially reduce the risk of cytokine storms in severe COVID-19 cases.
-Modulate immune signaling between lung epithelial cells and immune cells like monocytes.
However, the researchers caution that more studies are needed. Questions remain about how TLR10 interacts with other immune pathways and whether its immunosuppressive effects could impair antiviral defenses. Future research could also explore inhalable treatments that use TLR10 modulation to deliver targeted therapies directly to the lungs.
The study findings were published in the peer-reviewed journal: Frontiers in Immunology.
https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1490478/full
For the latest COVID-19 News, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/indian-study-unveils-protein-changes-in-lung-cells-in-response-to-sars-cov-2-orf3a
https://www.thailandmedical.news/news/covid-19-increases-the-risk-of-lung-cancer
https://www.thailandmedical.news/news/tlr2-and-tlr4-are-novel-activating-receptors-for-sars-cov-2-spike-protein-in-nk-cells
https://www.thailandmedical.news/articles/coronavirus