Human H5N1 Infections in America Rises to 36 With 387 Dairy Herds Affected Along with Hundreds of Poultry Farms Across 48 States!
Nikhil Prasad Fact checked by:Thailand Medical News Team Oct 30, 2024 5 months, 2 weeks, 18 hours, 38 minutes ago
Medical News: Bird Flu Outbreak Sweeps Across U.S.
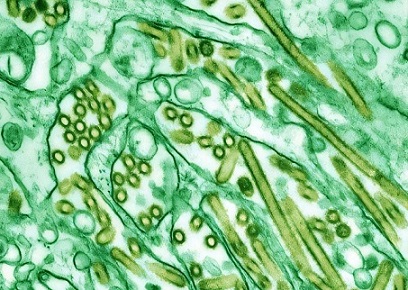
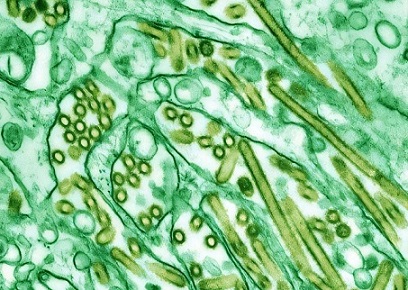
The United States is currently experiencing a significant outbreak of the H5N1 avian influenza virus, commonly known as bird flu. The infection count among humans has risen to 36 across several states, marking a worrying spread in both livestock and poultry. In addition to human cases, 387 dairy herds across 14 states and hundreds of poultry farms across 48 states are affected, escalating concerns over the economic and health impacts.
 Human H5N1 Infections in America Rises to 36 With 387 Dairy Herds Affected
Human H5N1 Infections in America Rises to 36 With 387 Dairy Herds Affected
Along with Hundreds of Poultry Farms Across 48 States
While authorities claim that they have the situation under control, the situation seems to be escalating with growing risk to the masses. There are hundred farmworkers who have yet to be tested and there are hundreds of suspected cases of H5N1 infections that have yet to be laboratory tested.
To make matters worse, a new more transmissible and possibly lethal strain of H5N1 virus has been detected in an infected Texas farmworker.
https://www.thailandmedical.news/news/a-more-transmissible-and-possibly-lethal-h5n1-strain-hutx37-h5n1-discovered-in-an-infected-farmworker-in-america
There is also growing concerns that while many of the initial human infections were deemed as mild, the mid to long-term health effects could be worrying especially on the human brain and CNS.
According to researchers from institutions including the U.S. Centers for Disease Control and Prevention (CDC), University of California, and Colorado State University, California has reported the highest number of human cases, with 16 individuals infected, all linked to farmworkers in the dairy industry. Genetic sequencing has confirmed that the H5N1 virus in these cases stems from the clade 2.3.4.4b subtype, which has shown a strong propensity for transmission among animals and humans. Other states, including Colorado and Washington, have also reported human cases, largely associated with poultry farmworkers. In total, California, Colorado, Missouri, Michigan, Texas, and Washington are dealing with human cases of this virus.
This
Medical News report highlights how the spread of the virus in livestock could pose potential risks for human-to-human transmission. Experts are monitoring these cases closely, particularly as flu season approaches in the U.S., where seasonal flu could compound the health threat posed by H5N1.
Rising Infections in Dairy and Poultry Farms
Since its emergence in dairy herds earlier this year, H5N1 has led to significant livestock fatalities, especially in California. In just the past 30 days, the number of affected dairy herds in the state has reached 186, causing severe economic strain on farms. With limited means for carcass disposal, many farmers are forced to leave deceased cattle
roadside, awaiting collection by overwhelmed authorities. The U.S. CDC estimates that the ongoing outbreak in cattle and poultry may soon have a lasting impact on both local and national agriculture, affecting both meat and dairy production.
Across the U.S., poultry farms in 48 states have been struck by the virus.
https://www.cdc.gov/bird-flu/situation-summary/index.html
According to Dr. Allen Rossman from Washington State University, “The current bird flu situation is disturbing and challenging to contain.” He notes that despite efforts, the virus continues to spread among animals, raising the probability of further human cases. The risk is particularly high in locations with a dense population of livestock and poultry, as these are ideal environments for avian influenza to mutate and potentially adapt to humans.
Human Cases: From Farmworkers to Unknown Sources
The U.S. CDC reports that, to date, the majority of human cases in California stem from dairy farmworkers exposed to infected cattle, while human cases in Colorado and Washington mostly involve poultry farmworkers. However, one concerning case in Missouri has an unidentified source of infection, suggesting the virus could be present in unmonitored environments. Health experts emphasize the importance of ongoing surveillance and strict biosecurity measures to limit exposure and prevent further infections.
In the most recent updates, farmworkers who tested positive have experienced only mild symptoms, primarily conjunctivitis (eye redness or discharge). While mild, these symptoms highlight the direct animal-to-human transmission risk. Given the highly mutative nature of influenza viruses, there is concern that if H5N1 undergoes further changes, it could gain the capacity for more efficient human-to-human transmission. As Dr. Rossman notes, “The more the virus spreads in animals and humans, the more opportunities it has to mutate and potentially develop transmissibility between humans.”
Current Risk Assessment and Surveillance
According to U.S. CDC data, there are currently no indicators of widespread transmission among humans. However, national flu surveillance programs are testing thousands of specimens weekly to monitor any signs of unusual flu activity. In the 2024 flu season alone, over 55,000 specimens have been tested for influenza A(H5) and other novel viruses. This targeted surveillance helps identify potential hotspots for H5N1 spread, especially among those with recent exposure to infected animals. As of now, over 6,100 individuals who have been exposed to infected animals are under surveillance, and around 300 have undergone testing.
The U.S. CDC advises that the risk of human-to-human transmission of H5N1 remains low, but notes that this assessment could change as the virus continues to circulate in animal populations. The U.S. CDC is also working closely with local health departments to ensure that any potential case clusters are quickly contained, with guidelines recommending isolation and treatment protocols for infected individuals.
Impact on Agriculture and Food Safety Measures
The H5N1 outbreak in both dairy and poultry farms has had significant economic repercussions. With hundreds of dairy herds and over 100 million poultry affected, farmers are facing mounting challenges. The U.S. Department of Agriculture (USDA) and the U.S. CDC have collaborated to implement strict biosecurity measures, encouraging farmers to avoid direct contact with wild birds, monitor livestock for signs of illness, and report any unusual animal deaths immediately. The USDA has also provided guidelines to ensure the safe handling of poultry products, assuring the public that properly cooked poultry remains safe to consume.
In terms of dairy, the U.S. CDC advises consumers to avoid raw milk and instead opt for pasteurized products, as pasteurization eliminates any potential viral presence. Local health authorities are also conducting checks at livestock markets and have restricted the movement of animals in affected areas to reduce the risk of spread. Although there is no immediate concern for milk and dairy products from affected herds, some states have temporarily restricted dairy imports from highly affected regions until the situation stabilizes.
Protective Actions and Public Health Recommendations
Health authorities are emphasizing the importance of protective actions around animals, especially in areas experiencing outbreaks. Farmers and farmworkers are advised to use personal protective equipment (PPE) when handling livestock and avoid unprotected physical contact with any animal suspected to be infected. Similarly, the U.S. CDC advises against handling dead birds or animals without gloves and recommends reporting any sightings of ill wildlife.
For those working directly with infected animals, the U.S. CDC has provided interim guidance to employers to help reduce risk. These guidelines focus on using protective equipment, implementing biosecurity measures, and ensuring prompt reporting of symptoms in both animals and humans. Seasonal flu vaccination, although not protective against H5N1, is encouraged as it reduces the risk of concurrent seasonal and avian flu infections.
Conclusion
The ongoing H5N1 outbreak across the United States underscores the delicate balance between agriculture, public health, and disease prevention. While the current risk of human-to-human transmission remains low, the steady increase in animal and human cases is a concerning trend. The outbreak highlights the need for robust monitoring systems, rapid containment measures, and close cooperation among federal, state, and local health authorities to minimize the risks to both human and animal populations.
Looking forward, health experts are calling for expanded biosecurity and surveillance protocols to prevent future outbreaks. It is crucial that farmers, agricultural workers, and the general public remain vigilant, as the virus could still pose a significant threat if it adapts to human hosts. The growing number of cases suggests that while animal-to-human transmission remains the primary pathway, the virus’s potential to evolve is ever-present. Maintaining awareness, following safety protocols, and reducing exposure to infected animals will be essential in keeping this outbreak contained.
For the latest H5N1 Bird Flu updates, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/human-h5n1-infections-in-america-now-rises-to-31-while-missouri-detects-second-case-mysterious-bird-flu-infection
https://www.thailandmedical.news/news/breaking-gut-molecule-indole-3-propionic-acid-ipa-shows-promise-in-fighting-all-types-of-influenzas