Human Leukocyte Antigen (HLA) and Its Role in Long COVID and Persistent Antigens
Nikhil Prasad Fact checked by:Thailand Medical News Team Feb 15, 2025 2 months, 12 hours, 18 minutes ago
Medical News: Recent research has revealed that some individuals who have recovered from COVID-19 continue to experience persistent symptoms long after the initial infection. Scientists have identified one major factor that may explain why certain people develop Long COVID while others do not: the role of Human Leukocyte Antigen (HLA) in the immune system’s response to SARS-CoV-2, the virus that causes COVID-19.
 Human Leukocyte Antigen (HLA) and Its Role in Long COVID and Persistent Antigens
Human Leukocyte Antigen (HLA) and Its Role in Long COVID and Persistent Antigens
The study was conducted by researchers from the Brain Sciences Center at the Minneapolis Veterans Affairs Health Care System, the Department of Neuroscience and Psychiatry at the University of Minnesota Medical School, and the Department of Medicine at the University of Minnesota Medical School-USA. Their work has provided a new perspective on how immune system genetics may contribute to the persistence of viral antigens in people suffering from Long COVID. In this
Medical News report, we explore the key findings of this study and what they mean for those affected by ongoing COVID-19 symptoms.
What is HLA and Why Does it Matter
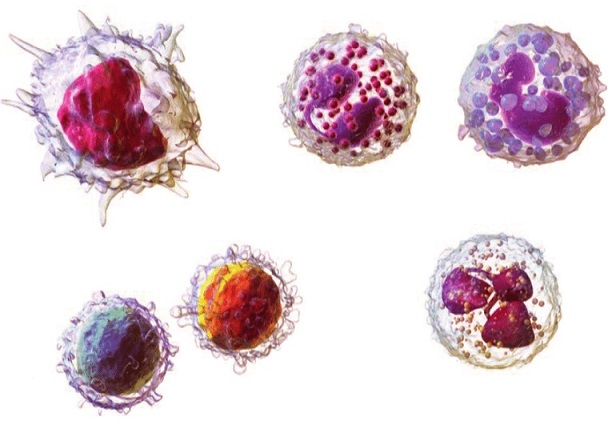
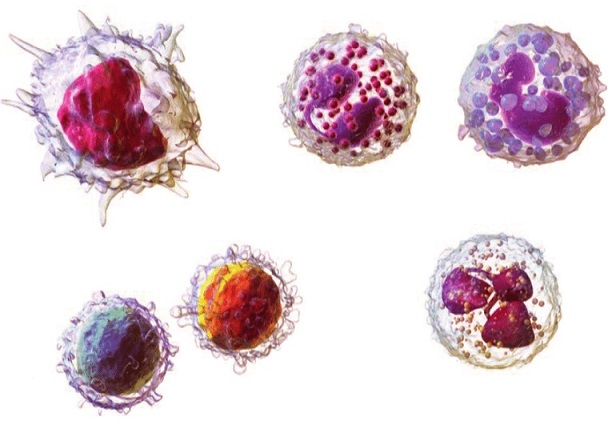
HLA is a group of molecules found in almost all cells of the human body. These molecules play a vital role in the immune system by helping the body recognize and eliminate harmful invaders such as viruses. HLA molecules present small fragments of these viruses to immune cells, signaling them to attack infected cells and stop the spread of infection.
The immune system has two main types of HLA-related defense mechanisms. The first is HLA Class I (HLA-I), which works by presenting viral proteins to cytotoxic T cells. These immune cells destroy infected cells within the first 10 days of an infection, preventing the virus from continuing to spread. The second mechanism is HLA Class II (HLA-II), which helps the body produce antibodies against foreign antigens. These antibodies neutralize the virus and provide long-term immunity.
However, the effectiveness of this immune response depends on an individual’s unique set of HLA genes. Since people inherit only six HLA-I and six HLA-II alleles from their parents, some individuals may have genetic variations that make them less effective at fighting SARS-CoV-2. This could lead to viral persistence and contribute to the development of Long COVID.
Persistent Antigens and Their Role in Long COVID
One of the key findings of this study is that SARS-CoV-2 antigens can remain in the body for months after the initial infection. Researchers found that some individuals still had viral antigens in their blood up to 14 months after recovering from COVID-19. This persistence of antigens is associated with post-acute sequelae of COVID-19 (PASC), commonly known as Long COVID.
Scientists believe that individuals with certain HLA genetic profiles may have a lower ability to form stable antigen-HLA complexes, which are necessary for triggering an effective immune response. If the immune system cannot effectively clear the virus, remnants of SARS-CoV-2 proteins may continue
to circulate in the body. These persistent antigens can cause ongoing inflammation and contribute to symptoms such as fatigue, brain fog, shortness of breath, and muscle pain - common complaints among Long COVID sufferers.
How Genetics Influence Immune Response to SARS-CoV-2
The study highlights how variations in HLA genes determine whether an individual can effectively eliminate the virus or if they remain vulnerable to persistent viral proteins. When an individual has HLA alleles with strong binding affinity to SARS-CoV-2 antigens, the immune system can successfully clear the infection. However, if the binding affinity is weak, the virus may not be effectively eliminated, leading to long-term symptoms.
This finding is important because it helps explain why some people experience mild or no symptoms after COVID-19, while others struggle with prolonged health issues. The researchers suggest that future studies should analyze the HLA profiles of Long COVID patients to determine if specific genetic markers are associated with prolonged antigen persistence.
Comparing Long COVID to Other Chronic Conditions
The study also draws comparisons between Long COVID and other chronic conditions linked to persistent antigens. Similar cases have been documented in diseases such as chronic Lyme arthritis and Gulf War Illness, where antigens from bacterial infections or vaccines remain in the body and trigger prolonged immune responses. Understanding how persistent antigens contribute to Long COVID could help scientists develop new strategies to treat or prevent these lingering symptoms.
Future Implications and Possible Interventions
One of the most promising outcomes of this research is the potential to use HLA profiling to predict an individual’s risk of developing Long COVID. By analyzing a person’s genetic makeup, doctors may be able to determine whether they have a strong or weak immune response to SARS-CoV-2. This information could be used to develop personalized treatment plans or identify individuals who may benefit from targeted immune therapies.
Additionally, the study suggests that future vaccines could be designed to take HLA binding affinities into account. Since vaccine effectiveness can vary based on an individual’s HLA profile, creating vaccines tailored to different genetic backgrounds may improve overall protection against COVID-19 and reduce the risk of persistent antigens.
Conclusion
The discovery that HLA genetics influence the persistence of SARS-CoV-2 antigens offers valuable insights into the underlying causes of Long COVID. Individuals with weak HLA binding affinities may struggle to clear the virus completely, leading to ongoing inflammation and chronic symptoms. By identifying these genetic factors, researchers hope to develop personalized medical approaches that can help prevent and treat Long COVID more effectively.
While much remains to be understood about Long COVID, this study represents an important step toward unraveling the complexities of post-viral syndromes. Future research will focus on identifying specific HLA variations that contribute to antigen persistence and exploring new therapeutic interventions to help those affected by lingering symptoms.
The study findings were published in the peer-reviewed Journal of Immunological Sciences.
https://www.immunologyresearchjournal.com/articles/human-leukocyte-antigen-hla-at-the-root-of-persistent-antigens-and-long-covid
For the latest COVID-19 News, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/american-study-finds-that-viral-superinfection-can-trigger-anti-hla-antibodies
https://www.thailandmedical.news/news/hla-b-21m-t-dimorphism-linked-to-reduced-covid-19-severity
https://www.thailandmedical.news/news/the-role-of-human-leukocyte-antigen-and-micrornas-in-alzheimer-s-disease
https://www.thailandmedical.news/pages/thailand_doctors_listings
Follow us on:
https://x.com/ThailandMedicaX
https://www.facebook.com/ThailandMedicalNews
https://bsky.app/profile/thailandmedical.bsky.social
https://gettr.com/user/thailandmedicalnews
https://www.tribel.com/thailandmedical/wall
and 33 other social media platforms