Nikhil Prasad Fact checked by:Thailand Medical News Team Jan 01, 2025 3 months, 1 week, 5 days, 2 hours, 31 minutes ago
HMPV News: Introduction to the Hidden Threat
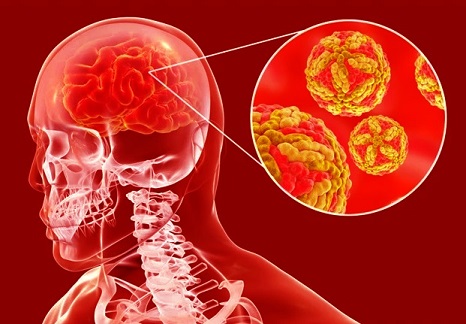
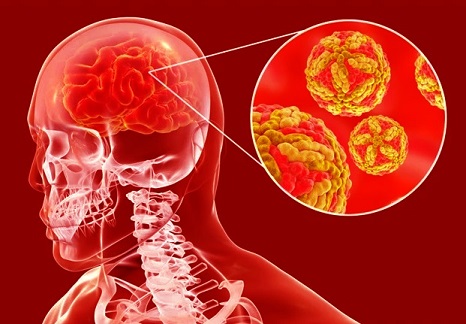
Human metapneumovirus (hMPV), a respiratory virus known for causing acute lower respiratory infections, has recently been implicated in causing damage beyond the lungs. A groundbreaking study from researchers at the Millennium Institute of Immunology and Immunotherapy, Pontificia Universidad Católica de Chile, has shed light on how hMPV can impact the central nervous system (CNS). This virus, primarily affecting infants, the elderly, and immunocompromised individuals, has now been linked to conditions like encephalitis and encephalopathy.
 Human Metapneumovirus (HMPV) Can Impair the Central Nervous System
Human Metapneumovirus (HMPV) Can Impair the Central Nervous System
The study, spearheaded by Alexis M. Kalergis, Karen Bohmwald, and Catalina A. Andrade, explores the neuroinvasive and neuroinflammatory mechanisms of hMPV. Using a robust experimental design, the team revealed that while viral particles may not directly infiltrate the brain, the infection sets off a cascade of immune responses that compromise neurological health. This
HMPV News report delves into the key findings, offering a glimpse into the broader implications of respiratory viruses on brain function.
Study Background and Objectives
Pneumoviruses, such as hMPV and the respiratory syncytial virus (RSV), have long been associated with respiratory distress. However, emerging evidence suggests that their impact extends to the CNS. The researchers aimed to uncover how these viruses influence brain function, focusing on inflammation, blood-brain barrier (BBB) integrity, and behavioral outcomes.
The study utilized a mouse model to compare the effects of hMPV and RSV infections. Mice were infected with either virus or treated with non-infectious controls (mock). Researchers then analyzed viral loads, cytokine levels, BBB permeability, and cognitive performance.
Key Findings on Neuroinflammation
Interestingly, while hMPV infection did not result in detectable viral loads in the brain, as seen with RSV, it triggered significant systemic inflammation. Pro-inflammatory cytokines such as interleukin-6 (IL-6) and interferon-gamma (IFN-γ) were markedly elevated in the serum of hMPV-infected mice. The brain tissue analysis further revealed distinct patterns of cytokine expression for both viruses. For hMPV, there were increases in IL-6, tumor necrosis factor-alpha (TNF-α), and interleukin-4 (IL-4). These findings underscore the role of immune-mediated mechanisms in CNS impairment.
Blood-Brain Barrier Disruption
Another critical discovery was the increased permeability of the BBB in mice infected with either virus. The BBB serves as a protective shield, preventing harmful substances from entering the brain. Its disruption allows inflammatory molecules to infiltrate the CNS, potentially leading to neuroinflammation and neuronal damage. This aspect of the study highlights a shared pathogenic pathway between hMPV and RSV despite differences in direct neuroinvasion.
Behavioral and Cognitive Implications
Weeks after t
he initial infection, the researchers assessed the mice's cognitive function using the Marble Burying (MB) test. This simple yet effective test evaluates repetitive and anxiety-related behaviors, providing insight into potential long-term neurological impacts. Mice infected with hMPV displayed impaired cognitive performance, similar to those infected with RSV. These behavioral changes suggest that even after the acute phase of infection, the effects on the CNS persist, potentially mirroring post-viral syndromes observed in humans.
Broader Implications of the Findings
This study provides compelling evidence that hMPV, traditionally viewed as a respiratory pathogen, has a profound impact on neurological health. The observed cognitive impairments in mice align with clinical reports of neurological symptoms in patients with severe hMPV infections. By identifying the inflammatory mediators involved, this research opens new avenues for therapeutic interventions aimed at mitigating CNS damage during respiratory virus infections.
Moreover, the findings raise questions about the potential long-term effects of repeated or chronic exposure to pneumoviruses. Could recurrent infections contribute to neurodegenerative diseases or cognitive decline in later life? These are critical issues warranting further exploration.
Conclusions and Future Directions
The study by Kalergis, Bohmwald, and Andrade offers a nuanced understanding of how respiratory viruses like hMPV can affect the brain. Their findings emphasize the importance of monitoring neurological symptoms in patients with severe respiratory infections, especially in vulnerable populations.
The disruption of the BBB and the role of pro-inflammatory cytokines provide actionable targets for future research. Therapeutics aimed at preserving BBB integrity or modulating cytokine responses could potentially prevent or reduce CNS complications.
The study also underscores the need for comprehensive patient care approaches that address both respiratory and neurological health. As the global burden of respiratory viruses continues to rise, integrating this knowledge into clinical practice will be essential for improving patient outcomes.
Final Thoughts
The evidence that hMPV can impair the CNS reshapes our understanding of respiratory viruses. This research highlights the intricate interplay between infection, immune response, and neurological health. While significant progress has been made, much remains to be done in unraveling the long-term consequences of pneumovirus infections on the brain.
The study findings were published in the peer-reviewed journal: The Journal of Immunology.
https://journals.aai.org/jimmunol/article/210/1_Supplement/236.22/263946/Pneumoviruses-can-impair-the-central-nervous
For the latest
HMPV News, keep on logging to Thailand Medical News.
Read Also:
https://www.thailandmedical.news/news/chilean-case-study-shows-that-human-metapneumovirus-hmpv-infections-can-cause-fatal-hemorrhagic-pneumonia
https://www.thailandmedical.news/news/columbia-university-study-finds-that-the-phytochemical-ginkgolic-acid-can-inhibit-human-metapneumovirus-infectivity
https://www.thailandmedical.news/news/emerging-novel-lineages-of-human-metapneumovirus-in-china-mark-the-start-of-2025
https://www.thailandmedical.news/news/understanding-the-human-metapneumovirus-incubation-period
https://www.thailandmedical.news/news/human-metapneumovirus-hmpv-can-cause-neurologic-issues
https://www.thailandmedical.news/news/scientists-from-chile-discover-that-human-metapneumovirus-infections-also-affect-both-innate-and-adaptive-intestinal-immunity
https://www.thailandmedical.news/news/israeli-study-finds-that-human-metapneumovirus-uses-unique-strategy-to-escape-recognition-by-nk-cells
https://www.thailandmedical.news/news/louisiana-study-finds-that-human-metapneumovirus-uses-mirnas-to-impair-immune-responses-involving-interferons
https://www.thailandmedical.news/news/human-metapneumovirus-infections-on-the-rise-in-china
https://www.thailandmedical.news/news/probenecid-shows-promise-against-respiratory-virus-human-metapneumovirus-hmpv
https://www.thailandmedical.news/articles/hmpv-human-metapneumovirus
Follow Us on:
https://x.com/ThailandMedicaX
https://bsky.app/profile/thailandmedical.bsky.social
https://www.facebook.com/ThailandMedicalNews
https://gettr.com/user/thailandmedicalnews
https://www.tribel.com/thailandmedical/wall