Nikhil Prasad Fact checked by:Thailand Medical News Team Nov 30, 2024 4 months, 1 week, 6 days, 6 hours, 56 minutes ago
Medical News: Researchers from the University of Foggia in Italy have revealed promising findings about the protective role of immunoglobulin A (IgA) in severe COVID-19 cases. The study focused on patients with acute respiratory failure caused by SARS-CoV-2 who were admitted to intensive care units (ICUs). By examining bronchoalveolar lavage (BAL) samples, the researchers aimed to identify correlations between IgA presence and patient outcomes, shedding light on the potential of mucosal immunity in combating severe respiratory infections.
 IgA Role in COVID-19 Recovery Among ICU Patients
The Study and Its Methods
IgA Role in COVID-19 Recovery Among ICU Patients
The Study and Its Methods
This
Medical News report highlights that the research team, including experts from the Department of Surgical and Medical Science and the Anesthesia and Intensive Care Unit at Policlinico Riuniti di Foggia, analyzed data from 57 patients. These patients, diagnosed with severe COVID-19, were admitted to the ICU between March and May 2021. BAL and plasma samples were collected and tested for the presence of SARS-CoV-2-specific IgA and IgG antibodies using an enzyme-linked immunosorbent assay (ELISA).
The researchers found IgA antibodies in 19 out of 40 BAL samples and IgG in only one. Interestingly, none of the patients with detectable IgA in their BAL samples succumbed to the disease, highlighting the potential role of this antibody in survival. This contrasted sharply with patients who lacked IgA in BAL samples, seven of whom died during the study period.
Key Findings on IgA's Role
The study demonstrated a clear correlation between the presence of IgA in the lungs and better survival outcomes. Patients with IgA in their BAL samples were more likely to recover from severe respiratory distress compared to those without. These findings point to the importance of mucosal immunity, particularly IgA, in controlling and neutralizing the virus within the respiratory tract.
The study also revealed that patients with lower APACHE II and SOFA scores, which measure the severity of disease and organ failure, were more likely to have detectable IgA. Age also played a significant role; older patients were less likely to have IgA in their BAL samples. This suggests that age-related immune response decline may impact the production of protective antibodies like IgA.
Implications for Treatment and Vaccine Development
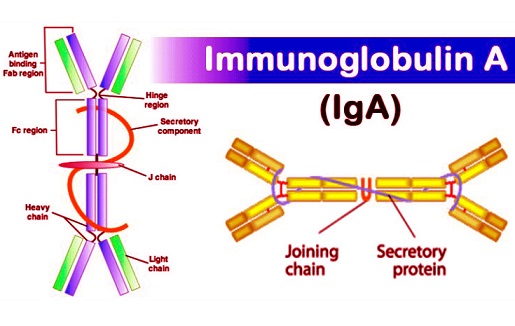
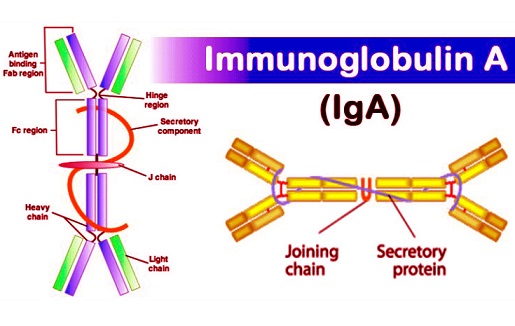
The findings highlight IgA's potential as a therapeutic target. Mucosal IgA is known to neutralize pathogens and prevent their attachment to epithelial cells, making it a critical line of defense against respiratory viruses like SARS-CoV-2. The study opens avenues for developing IgA-based therapies and vaccines that specifically enhance mucosal immunity.
Intranasal vaccines or treatments designed to boost IgA production in mucosal tissues could provide localized protection against respiratory infections. The protective effect of IgA in BAL samples underscores its importance in preventing viral replication and improving clinical outcomes in severe COVID-19 cases.
&nb
sp;
Broader Context of IgA in COVID-19
Previous research has also indicated that individuals with selective IgA deficiency are more prone to severe COVID-19 and reinfections, further emphasizing the antibody's protective role. Additionally, IgA's ability to act at mucosal surfaces, where respiratory viruses first establish infection, makes it a valuable tool in the fight against COVID-19 and other similar diseases.
Despite its promising role, the study acknowledges certain limitations, including the relatively small sample size and the focus on patients in a single ICU. Variations in viral strains, patient demographics, and treatment protocols may also influence the findings.
Conclusions and Future Directions
The study conducted by the University of Foggia underscores the critical role of IgA in improving survival among severe COVID-19 patients. By highlighting the inverse relationship between IgA presence in BAL samples and mortality, the research points to the potential of leveraging mucosal immunity in treatment strategies.
Future research should focus on larger, more diverse patient populations to validate these findings. Investigating how to effectively induce IgA production, whether through vaccines or other immunotherapies, could revolutionize respiratory disease management. Moreover, understanding the interplay between systemic and mucosal immunity in COVID-19 could provide insights into optimizing treatment and prevention strategies.
The study findings were published in the peer-reviewed journal: Viruses.
https://www.mdpi.com/1999-4915/16/12/1851
For the latest COVID-19 News, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/covid-19-causes-sugar-modifications-of-iga-which-in-turn-contributes-to-netosis
https://www.thailandmedical.news/news/post-covid-19-individuals-with-iga-nephropathy-found-to-have-overactivated-complement-system