Immune Dysregulation And Prolonged Disease Course In COVID-19 Patients Coinfected With Mycobacterium Tuberculosis Or HIV
Nikhil Prasad Fact checked by:Thailand Medical News Team Feb 25, 2024 1 year, 10 months, 1 week, 2 days, 3 hours, 12 minutes ago
COVID-19 News: The ongoing global pandemic caused by the novel coronavirus, SARS-CoV-2, has led to extensive research on its various aspects. Among the emerging insights is the impact of coinfections on disease severity and immune response. This
COVID-19 News report delves into a comprehensive study conducted at The First Affiliated Hospital of Zhengzhou University in China, exploring the immune dysregulation in SARS-CoV-2 patients coinfected with Mycobacterium tuberculosis (Mtb) or Human Immunodeficiency Virus (HIV).
 Immune Dysregulation in SARS-CoV-2 patients coinfected with Mycobacterium tuberculosis (Mtb) or HIV
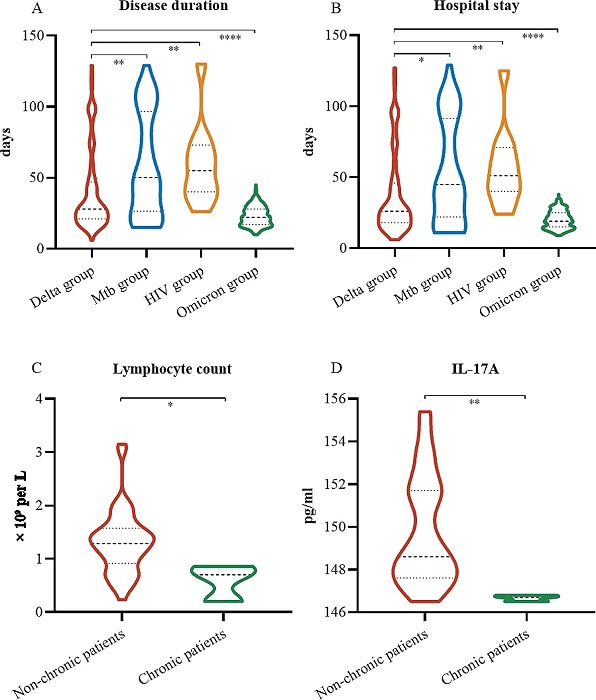
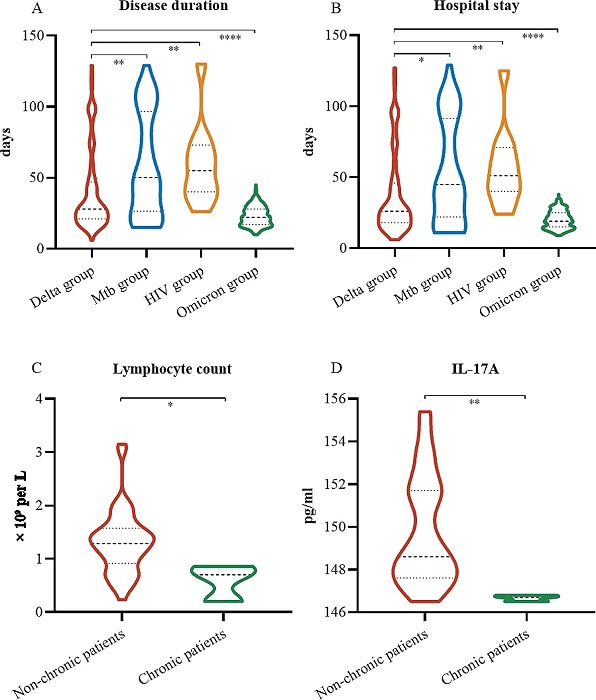
Disease duration and hospital stay for three groups of Delta-infected patients. (A) Disease duration in the four groups. (B) LOS in the four groups. (C) Comparison of the serum levels of IL-17 A between the nonchronic and chronic groups in the Mtb group. (D) Comparison of lymphocyte counts between the nonchronic and chronic groups in the Mtb group. *, P <.05; **, P <.01; ***, P <.001; ****, P <.0001; ns, not significant
Background
Immune Dysregulation in SARS-CoV-2 patients coinfected with Mycobacterium tuberculosis (Mtb) or HIV
Disease duration and hospital stay for three groups of Delta-infected patients. (A) Disease duration in the four groups. (B) LOS in the four groups. (C) Comparison of the serum levels of IL-17 A between the nonchronic and chronic groups in the Mtb group. (D) Comparison of lymphocyte counts between the nonchronic and chronic groups in the Mtb group. *, P <.05; **, P <.01; ***, P <.001; ****, P <.0001; ns, not significant
Background
SARS-CoV-2 infections are known to induce immune dysregulation in the human body. However, limited research has focused on understanding the immunological changes resulting from coinfections with Mtb or HIV. The study aims to shed light on these coinfections and their implications on clinical outcomes.
Methods
The researchers conducted a retrospective study involving 550 patients infected with SARS-CoV-2. The patients were categorized into four groups based on the presence of coinfections: Delta-infected patients with no coinfections, Delta-Mtb coinfections, Delta-HIV coinfections, and Omicron-infected patients. Various parameters such as epidemiologic information, laboratory findings, treatments, and clinical outcomes were collected and analyzed.
Results
Epidemiological Characteristics:
The Delta-Mtb and Delta-HIV groups showed a higher percentage of males (71% and 73%, respectively). In the Delta group, the median age was 41 years, with 27% associated with family clusters. The Omicron group had a higher proportion of patients aged less than 18 years (61%) and those who completed two doses of the COVID-19 vaccine (90%).
Clinical Features
Patients in the Delta group exhibited underlying diseases, including diabetes, hypertension, and cardiovascular disease. Myalgia or fatigue was more prevalent in the Delta-Mtb and Delta-HIV groups. The Omicron group showed a shorter incubation period and time from symptom onset to hospital admission.
Laboratory Abnormalities
Compared to the Delta group, the Delta-Mtb and Delta-HIV groups exhibited lower white blood cell co
unts and lymphopenia. Chest CT findings were abnormal in more than half of the patients in these groups. The Omicron group showed changes in various laboratory parameters.
Lymphocyte Subpopulations and Cytokines
The Delta-Mtb group had significantly lower total T-cell, CD4+ T-cell, CD8+ T-cell, and B-cell counts compared to the Delta group. The Delta-HIV group showed lower CD4+ T-cell and B-cell counts but higher CD8+ T-cell counts. No significant differences in cytokines were observed among the groups.
Treatment and Clinical Outcomes
Most patients received traditional Chinese medicine and immunotherapy. The Delta-Mtb and Delta-HIV groups exhibited longer disease duration and length of hospital stay (LOS) compared to the Delta group. All patients were discharged, and no deaths occurred.
Unvaccinated Delta-Infected Patients
Analysis of unvaccinated Delta-infected patients in the Mtb and HIV groups showed lower B-cell and CD4+ T-cell counts. However, there was no significant difference in LOS or disease duration, suggesting that vaccination may impact disease severity.
Pediatric Patients
Pediatric patients in the Omicron group had milder symptoms, and cough was more common. D-dimer levels were higher in the Delta group, and LOS and disease duration were longer.
Chronic Disease Course
Three patients in the Delta-Mtb group exhibited a chronic disease course of more than four months, indicating a prolonged infection. These patients showed lower plasma concentration of IL-17 A, suggesting potential dysfunction of the Th17 cell response.
Discussion
The study emphasizes the impact of coinfections with Mtb or HIV on SARS-CoV-2 patients, leading to a longer disease duration and LOS. The decrease in B-cell and CD4+ T-cell counts indicates a relationship between these cells and immune function. The study also identifies a chronic course of SARS-CoV-2 infection in patients coinfected with Mtb, lasting more than four months.
Conclusion
In conclusion, the comprehensive study conducted at The First Affiliated Hospital of Zhengzhou University highlights the immune dysregulation and prolonged disease course in SARS-CoV-2 patients coinfected with Mtb or HIV. Understanding the intricate dynamics of these coinfections is crucial for developing effective treatment strategies and managing the ongoing global health crisis. The findings contribute valuable insights into the clinical characteristics and outcomes associated with SARS-CoV-2 coinfections, providing a foundation for future research and public health interventions.
The study findings were published in the peer reviewed journal: BMC Public Health.
https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-024-17905-3
For the latest
COVID-19 News, keep on logging to Thailand Medical News.