Source: Thailand Medical News Jan 15, 2020 5 years, 2 months, 2 weeks, 5 days, 13 hours, 39 minutes ago
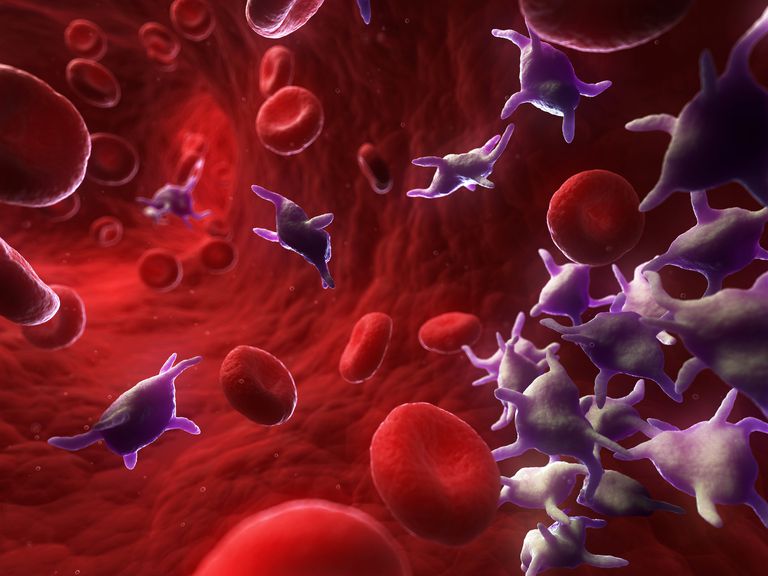
Study led by researchers at The Ohio State University Comprehensive
Cancer Center—Arthur G. James
Cancer Hospital (OSUCCC—James) reveals how a
clotting protein and blood
platelets can promote
cancer progression and suppress
immune responses to
cancer.
The study findings show how
thrombin, a
clotting protein in the blood, causes blood
platelets to release transforming growth factor-beta 1 (
TGF-b1), which is known for promoting disease progression in breast, prostate, colorectal and other
cancers, and for suppressing immune-system responses to
cancer.
Furthermore,
TGF-b1 is a leading cause for the failure of
immune therapies such as PD1 inhibitors in
cancer patients. This study may offers a new explanation for what causes tumors to resist immune therapies and become sensitive to the therapeutic agents.
The
cancer researchers used animal models to show that inhibiting
thrombin activity prevents the release of
TGF-1b and makes tumors that were resistant to anti-PD-1 immunotherapy susceptible to these agents.
The research findings are reported in the journal
Science Translational Medicine.
Principal investigator Dr Zihai Li, MD, Ph.D., a Professor in the Division of Medical Oncology at Ohio State and the founding director of the Pelotonia Institute for Immuno-Oncology (PIIO) at the OSUCCC—James told
Thailand Medical News, "In this study, we describe a direct connection between
thrombin and
TGF-b1, a cytokine that promotes tumor progression and suppresses the ability of
immune cells to attack the tumor. We also show that systemically interfering with this mechanism prevents the release of
TGF-1b and leads to changes in the tumor microenvironment that are favorable to anticancer
immune responses."
Dr Li, who is a member of the OSUCCC—James Translational Therapeutics Program also holds the Klotz Memorial Chair in Cancer Research at The Ohio State University College of Medicine
Dr Li notes that
cancer is similar to an unhealed wound that constantly activates the coagulation pathway and generates high concentrations of
thrombin in and around a tumor. That, in turn, causes chronic
platelet activation and release of
TGF-1b.
Dr Li added, "TGF plays important roles in
cancer development. Specifically,
TGF-b1 alters the tumor microenvironment in ways that protect
cancer cells from atta
ck by immune cells."
New research has shown that inhibiting
TGF-b1 enhances
cancer immunotherapy.
Dr Li further adds. "If we can effectively inhibit
TGF-b1 maturation or function, it should open new avenues for
cancer therapy."
In this research study, Li and his colleagues used blood samples from
cancer patients, genetic analyses, cell lines and animal models to investigate the mechanism underlying the release of mature
TGF-1b and the implications of blocking that release as a means of
cancer immunotherapy.
Major research findings include the following:
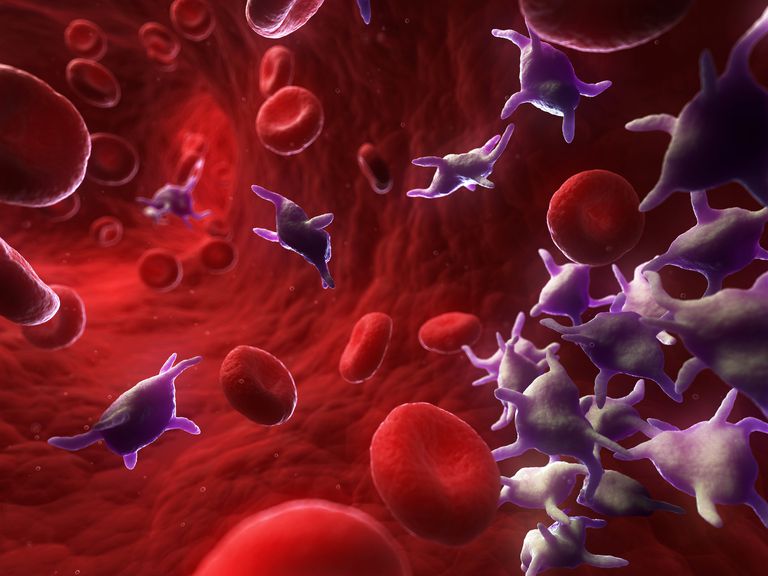
-Thrombin cleaves a molecule called GARP (glycoprotein A repetitions predominant) that is found on the surface of platelets;
-GARP cleavage leads to the release of mature
TGF-1b from
platelets;
-This cleavage is required to activate platelet
TGF-b1;
-Blocking
thrombin using the inhibitor dabigatran etexilate greatly altered the tumor microenvironment and increased the number and activity of tumor-infiltrating T cells, natural killer cells and neutrophils.
Dr Li concluded, "Overall, our study reveals a mechanism of
cancer immune evasion that involves
thrombin-mediated GARP cleavage and the release of
TGF-b1 by
platelets. It also suggests that blocking GARP cleavage could be an effective therapeutic strategy for overcoming
cancer's resistance to immunotherapy."
Reference: Alessandra Metelli et al. Thrombin contributes to cancer immune evasion via proteolysis of platelet-bound GARP to activate LTGF-β, Science Translational Medicine (2020). DOI: 10.1126/scitranslmed.aay4860