Nikhil Prasad Fact checked by:Thailand Medical News Team Mar 05, 2024 1 year, 7 months, 1 week, 5 days, 8 hours, 40 minutes ago
COVID-19 News: In the ongoing fight against the COVID-19 pandemic, understanding the intricacies of the immune response has become paramount. One fascinating aspect under intense scrutiny is the role of T cell cross-reactivity – a phenomenon where pre-existing memory T cells, generated in response to diverse infections or vaccinations, exhibit the ability to recognize and mount a response against SARS-CoV-2. This
COVID-19 News report delves into the intricate world of T cell cross-reactivity, shedding light on its mechanisms, impact on COVID-19 outcomes, and potential for cross-protection based on a study by researchers from School of Clinical Sciences, Monash University-Australia.
 Mechanism of TCR-dependent T cell cross-reactivity with SARS-CoV-2
Adaptive Immune Response to SARS-CoV-2
Mechanism of TCR-dependent T cell cross-reactivity with SARS-CoV-2
Adaptive Immune Response to SARS-CoV-2
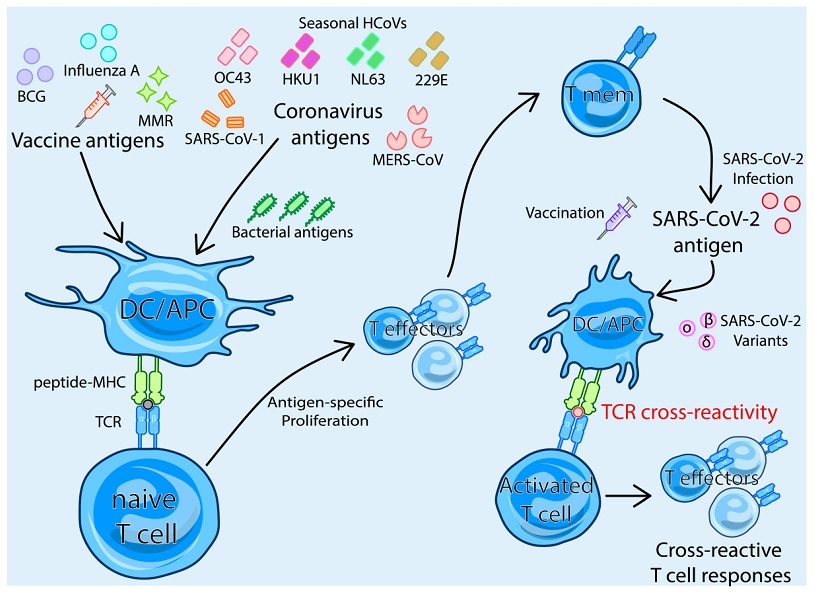
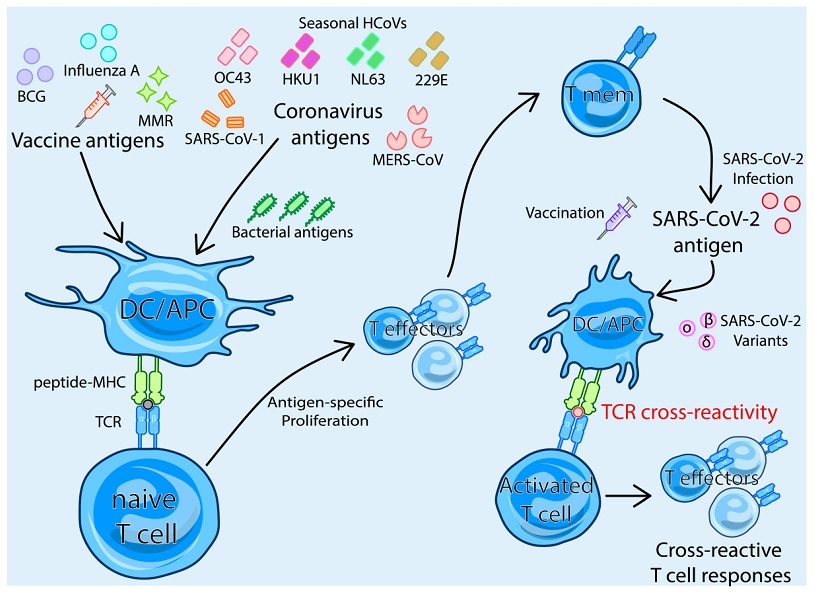
The Betacoronavirus SARS-CoV-2, responsible for COVID-19, triggers a sophisticated immune response in infected individuals. The adaptive immune system, particularly T cells, plays a pivotal role in combating the virus. CD8+ cytotoxic T cells and CD4+ T cells, crucial components of the adaptive immune response, work in harmony to clear the virus and influence the severity of COVID-19 outcomes.
Antigen-Specific T cell Responses to SARS-CoV-2
The adaptive immune response to SARS-CoV-2 is antigen-specific, driven by the recognition of viral epitopes presented by major histocompatibility complex (MHC) molecules. The SARS-CoV-2-specific T cells, predominantly CD4+, recognize epitopes across various viral proteins, with spike antigens dominating CD4+ and CD8+ T cell responses. Following infection or vaccination, these T cells transition into memory T cells, exhibiting robust, long-lasting immunity.
T Cell Cross-Reactivity: An Overview
T cell cross-reactivity can occur through T cell receptor (TCR)-dependent mechanisms, where memory T cells generated in response to one pathogen can recognize and respond to a different, unrelated pathogen. This cross-reactivity has been a subject of extensive research, especially concerning its role in COVID-19 outcomes.
-T Cell Cross-Reactivity and Cross-Protection between SARS-CoV-2 and Other Human Coronaviruses
Early evidence highlighted cross-reactive T cells between SARS-CoV-2 and common human coronaviruses (HCoVs) like OC43, HKU1, NL63, and 229E. These seasonal coronaviruses, prevalent in the human population, share amino acid sequence homology with SARS-CoV-2, leading to the potential for cross-reactive T cell responses. However, debates persist regarding the functional efficacy of these cross-reactive T cells, with studies indicating that low avidity may correlate with severe COVID-19 outcomes.
While cross-reactive T cells from HCoVs may not always offer robust protection, they demonstrate potential in reducing the severity of COVID-19. Notably, cross-reactive T cells against the nucleocapsid protein have shown promise in conferring protection, suggesting a time-dependent effect and paving the way for pan-coronavirus vac
cines that leverage non-spike epitopes.
-T Cell Cross-Reactivity between SARS-CoV-2 and Novel Variants
As novel variants of SARS-CoV-2 emerged, concerns arose regarding the potential evasion of pre-existing immunity. While humoral immunity showed decreased efficacy against some variants, memory T cells remained largely unaffected, underscoring their importance in maintaining protection against severe COVID-19 outcomes. Cross-reactive T cells demonstrated resilience against variants, contributing to over 88% protection against severe disease up to 40 weeks after initial infection, regardless of the variant responsible.
T Cell Cross-Reactivity from Different Vaccines or Pathogens
T cell cross-reactivity extends beyond HCoVs, encompassing a diverse range of sources, including vaccines and other pathogens. Exploring cross-reactivity from the Bacillus Calmette–Guérin (BCG) vaccine, influenza, the measles, mumps, and rubella (MMR) vaccine, as well as microbial antigens, reveals a complex interplay of memory T cells and their potential influence on COVID-19 outcomes.
-BCG Vaccine: Early in the pandemic, BCG vaccination demonstrated potential heterologous effects, offering protection against COVID-19. Cross-reactive T cells from BCG vaccination, especially CD4+ and CD8+ memory T cells, exhibited enhanced responses when exposed to SARS-CoV-2, suggesting a potential for improved COVID-19 outcomes.
-Influenza Vaccine: Association between high influenza vaccination coverage and reduced SARS-CoV-2 infection rates prompted investigations into cross-reactive T cells. Shared TCR clonotypes and functional cytokine responses between SARS-CoV-2 and influenza A virus epitopes suggest a potential role for influenza vaccination in influencing the immune response to COVID-19.
-MMR Vaccine: Studies linking the MMR vaccine to better COVID-19 outcomes revealed shared TCR clonotypes with SARS-CoV-2-vaccinated or convalescent individuals. Sequence homologies between MMR surface proteins and the SARS-CoV-2 spike further supported the notion of cross-reactive T cell responses contributing to cross-protection.
-Microbial Antigens: Cross-reactive memory T cells originating from exposure to microbial antigens, both pathogenic and commensal, exhibited homologies with SARS-CoV-2 epitopes. This opens avenues for exploring the contribution of unrelated pathogens to the overall cross-reactive T cell response in COVID-19.
Conclusions and Future Directions
The landscape of T cell cross-reactivity in the context of COVID-19 is dynamic and multifaceted. While evidence suggests the presence of cross-reactive T cells from various sources, further research is essential to unravel their precise impact on clinical outcomes. Understanding the correlation between cross-reactive T cells and protection against severe COVID-19, as well as elucidating the interplay with other immune cells, remains crucial. As the scientific community continues to explore these avenues, the insights gained may contribute to more effective strategies for combating not only SARS-CoV-2 but also potential future coronaviruses.
The study findings were published in the peer reviewed journal: Biomedicines.
https://www.mdpi.com/2227-9059/12/3/564
For the latest
COVID-19 News, keep on logging to Thailand Medical News.