Influenza News: University Of Chicago Study Shows That Pre-Existing Flu Immunity Affects Antibody Quality Following Vaccination Or Infection
Source: Influenza News Dec 13, 2020 5 years, 3 weeks, 4 days, 6 hours, 35 minutes ago
Influenza News: A new study by researchers from the University of Chicago suggests that an individual’s antibody response to influenza viruses is dramatically shaped by their pre-existing immunity, and that the quality of this response differs in individuals who are vaccinated or naturally infected. The study team found that infection-induced antibodies reacted to non-neutralizing epitopes of influenza virus, whereas vaccination-induced antibodies reacted to neutralizing epitopes. In addition, infection-induced antibodies preferentially responded to influenza strains present during an individual’s childhood.
The study findings demonstrated that existing influenza-specific memory and route of exposure influences influenza immunity.
The study results highlight the importance of receiving the annual flu vaccine to induce the most protective immune response.
The research findings were published in the peer reviewed journal: Science Translational Medicine.
https://stm.sciencemag.org/content/12/573/eabd3601
The study team found that most of the initial antibodies stimulated after both influenza infections and influenza vaccinations came from old B cells ie a type of white blood cell that secretes antibodies, indicating the immune system's memory plays a major role in how the body responds early on to a viral infection. These antibodies displayed higher reactivity toward strains of influenza that circulated during an individual's childhood compared to more recent strains.
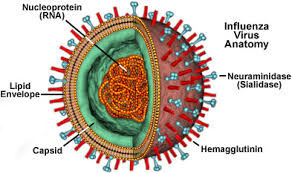
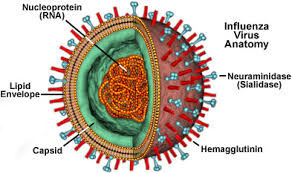
The research findings providesthose working on a universal influenza vaccine further understanding of how pre-existing immunity affects the development and performance of neutralizing and non-neutralizing antibodies following infection and vaccination. Any effective universal influenza vaccine will depend on scientists identifying 'conserved' parts of the influenza virus that do not mutate over time and that antibodies can target to prevent infection.
Dr Haley Dugan, co-first author of the study and a Ph.D. candidate in immunology told Thailand Medical News, "Most interestingly, we found that people who were actively sick with influenza had old antibodies that predominantly targeted parts of the virus that don't change but those antibodies specifically targeted non-neutralizing sites. When we tested these same antibodies in mice, they weren't able to protect them from being infected with influenza."
The study team found In contrast that influenza vaccinations boost antibodies that tended to target conserved yet neutralizing regions of the virus, which suggests vaccinations can draw upon pre-existing immunity to prompt more protective responses.
Interestingly vaccinated individuals also generated many antibodies that targeted new and mutated regions on the virus, suggesting these vaccine-induced antibodies are more adaptable.
The immune system memory ensures a rapid and specific response to previously encountered pathogens. Vaccinations work by exposing the immune system to a small amount of virus, which causes B cells to develop a biological memory to the virus. If the
body encounters the same virus later, the immune system is alerted to attack and eliminate the virus.
However in order to be protected, the viral proteins of the infecting strain must typically match those of the strain used in the vaccine. The memory B cells are like keys that fit and bind to the locks ie the viral proteins. These memory B cells can survive for decades, providing long-lasting protection from future infections.
However if the virus mutates and is significantly different, the memory B cells can no longer recognize the viral proteins, potentially leading to infection.
Importantly for this reason, the human body is pitted in an evolutionary arms race with the flu. Because influenza viruses rapidly evolve and mutate each season, our immune system has trouble recognizing the viral surface proteins on new influenza strains.
Hence our bodies often rely on old antibodies to fight new influenza strains; this is possible because some parts of the influenza virus that are critical to its structure or function do not change, remaining familiar to our immune system.
Scientists now understand that specific structural and functional parts of the influenza virus that do not change are better for antibodies to target than others. Antibodies that bind to one of these neutralizing sites are able to prevent infection, while antibodies that target non-neutralizing sites often cannot.
Researchers believe a person's age, history of exposure to the influenza virus and type of exposure either through infection or vaccination all shape whether their immune system antibodies target neutralizing or non-neutralizing sites on a virus.
For this research, the study team sought to address a major knowledge gap: Which conserved viral sites are preferentially targeted following natural infection versus vaccination in people, and how does pre-existing immunity play a role in shaping the landscape of neutralizing and non-neutralizing antibodies?
Co-first author and Immunology postdoctoral fellow Jenna Guthmiller, Ph.D. commented, "For individuals who have caught the flu, their pre-existing immunity may make them susceptible to infection or increase the severity of their influenza symptoms if their antibodies are targeting 'bad' or non-neutralizing viral sites."
Vaccination by contrast, largely induces neutralizing and protective antibodies, old and new, highlighting the importance of receiving the seasonal influenza vaccine.
Dr Patrick Wilson, Ph.D., a professor of immunology and lead author of the study added, "This study provides a major framework for understanding how pre-existing immunity shapes protective antibody responses to influenza in humans. We need more studies to determine whether the targeting of specific neutralizing and non-neutralizing viral sites directly impacts a person's likelihood of becoming ill."
The study team are now examining how early exposure to the influenza virus in children shapes their immune response later in life as a follow-up to this work.
The study team concluded, “The study findings reveal that both preexisting immunity and exposure type shape protective antibody responses to conserved influenza virus epitopes in humans. Natural infection largely recalls cross-reactive memory B cells against non-neutralizing epitopes, whereas vaccination harnesses preexisting immunity to target protective HA epitopes.”
For more
Influenza News, keep on logging to Thailand Medical News.